
Before my hypothyroidism diagnosis, I frequently relied on acid blockers like Tums and Zantac to manage heartburn. Over time, I began experiencing symptoms like low energy, weight gain, and hair loss, without realizing that my dependence on these medications might have contributed to my thyroid decline. It wasn’t until I connected the dots between prolonged acid blocker use and my thyroid issues that I understood the potential harm.
Acid blockers are commonly prescribed to alleviate acid reflux and heartburn, and many people take them daily. Medications like Omeprazole, Zantac (ranitidine), and famotidine offer short-term relief, but their long-term use can pose serious risks, especially for individuals with thyroid conditions. Millions of people take both thyroid medications, such as Levothyroxine and acid blockers simultaneously, often unaware of the dangers of this combination.
In this article, we explore how acid blockers can negatively impact thyroid health by interfering with the absorption of thyroid medication and contributing to nutrient deficiencies.
Understanding Acid Blockers
Acid blockers, such as proton pump inhibitors (PPIs) like Omeprazole and H2 blockers like Zantac, are commonly prescribed to reduce stomach acid production. These medications are used to treat conditions like gastroesophageal reflux disease (GERD), heartburn, stomach ulcers, and gastrointestinal bleeding. While effective at alleviating symptoms, acid blockers only address the symptoms, not the root causes of these conditions. Acid reflux occurs when stomach acid flows back into the esophagus, irritating its lining. If untreated, it can lead to serious complications such as Barrett’s esophagus or even esophageal cancer.
Acid blockers reduce the corrosive effects of acid on the esophagus, providing relief. However, their long-term use may create dependency, as they don’t address underlying issues, such as weak lower esophageal sphincters or dietary habits. While these medications offer temporary relief, they can negatively affect digestion and overall health. Stomach acid plays a crucial role in breaking down food, absorbing nutrients, and maintaining a healthy balance of bacteria. When acid blockers suppress acid production over extended periods, they disrupt digestion, lead to nutrient malabsorption, and increase the risk of gut infections.
These effects can exacerbate nutrient deficiencies in individuals with thyroid conditions, further impairing thyroid health. Because of these potential side effects, it is essential for individuals to carefully evaluate the long-term use of acid blockers. If symptoms persist, considering lifestyle changes, natural remedies, and addressing the underlying causes of acid reflux may offer more sustainable relief.
Importance of Stomach Acid
Stomach acid plays an essential role in maintaining a healthy digestive system. It helps break down food, especially proteins, and activates enzymes that assist in digestion. Food cannot be properly digested without enough stomach acid, leading to problems such as bloating, indigestion, and nutrient deficiencies. Stomach acid can also compromise the body’s ability to fight harmful bacteria, as it acts as a defense mechanism, preventing the growth of pathogens in the digestive tract.
One of the most critical functions of stomach acid is absorbing key nutrients like calcium, magnesium, iron, and vitamin B12. These nutrients are vital for many bodily functions, including maintaining bone health, supporting thyroid function, and ensuring proper immune response. Low stomach acid levels, often a side effect of long-term acid blocker use, can lead to nutrient deficiencies, increasing the risk of conditions like osteoporosis, anemia, and thyroid dysfunction. In addition to aiding digestion and nutrient absorption, stomach acid helps maintain a balanced gut microbiome.
When acid levels are too low, it creates an environment where harmful bacteria can thrive, leading to conditions like small intestinal bacterial overgrowth (SIBO). This imbalance can cause further digestive discomfort and weaken the immune system over time. Maintaining adequate stomach acid levels is critical for overall health, especially for individuals with digestive or thyroid concerns.
Impact of Acid Blockers on the Digestive System
Acid blockers are commonly used to manage symptoms like heartburn and acid reflux, but their long-term use can disrupt the digestive system in significant ways. While they provide short-term relief, one of the most concerning side effects is the alteration of the gut’s natural balance, leading to a disrupted microbiome. Stomach acid plays a crucial role in controlling the growth of harmful bacteria in the gut.
When its production is reduced, harmful bacteria can proliferate, leading to conditions such as small intestinal bacterial overgrowth (SIBO) and Clostridium difficile colitis, a serious infection of the intestines. Long-term use of acid blockers can also lead to nutrient malabsorption. Calcium, magnesium, iron, and vitamin B12 all require sufficient stomach acid for proper absorption. Without adequate stomach acid, the body struggles to absorb these essential nutrients, potentially resulting in deficiencies with serious health consequences. For example, calcium deficiency can weaken bones and increase fracture risk, while vitamin B12 deficiency can lead to cognitive decline and anemia. These deficiencies are particularly concerning for individuals with thyroid disorders, as proper thyroid function relies on these nutrients.
Beyond nutrient absorption, acid blockers are associated with increased risks of other serious conditions. Studies have shown that the contaminant N-nitrosodimethylamine (NDMA) in Zantac is a probable carcinogen. Even proton pump inhibitors (PPIs) like Omeprazole, when used long-term, have been linked to an increased risk of stomach cancer, chronic kidney disease, and bone fractures. For these reasons, it’s crucial to carefully weigh the risks and benefits of using acid blockers over extended periods. Exploring alternative treatments and lifestyle modifications may offer safer, long-term solutions. If you are using acid blockers, it’s worth discussing with your healthcare provider whether other options could reduce your dependence on these medications and mitigate potential health risks.
1. Impact of Acid Blockers on Acid Production, Gut Health, and Nutrient Absorption
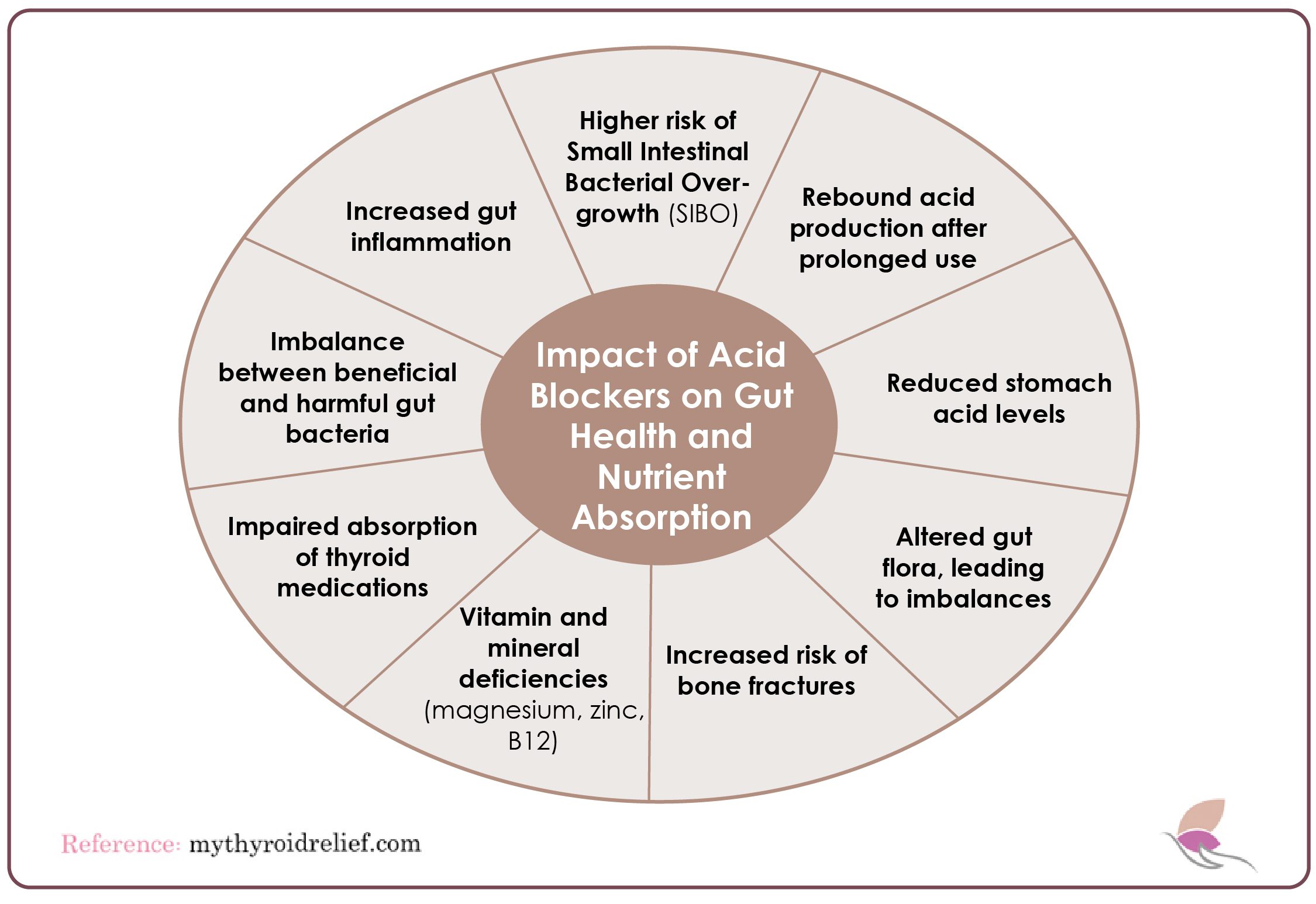
While acid blockers can provide short-term relief from acid reflux, their long-term use can cause a range of negative side effects. These effects are especially concerning for those who rely on them regularly. Some of the most significant issues include:
- Rebound Acid Production: After prolonged use, stopping acid blockers can cause the stomach to overproduce acid, leading to severe acid reflux. This creates a cycle of dependence on the medication as the body overcompensates.
- Altered Gut Flora: Acid blockers impair the stomach’s ability to maintain a healthy balance of bacteria. This disruption increases the risk of harmful bacteria proliferating, which can weaken the immune system and contribute to digestive issues.
- Increased Risk of Bone Fractures: Long-term use of acid blockers is linked to reduced calcium absorption, weakening bones and increasing the risk of fractures, especially in the hips.
Given these risks, it is essential to carefully evaluate the long-term use of acid blockers and consider alternative treatments. Consulting with a healthcare provider can help assess specific needs and avoid potential complications.
2. Nutrient Deficiencies and Thyroid Health
Nutrient deficiencies caused by acid blockers can be particularly challenging for individuals with thyroid conditions. Magnesium, iron, zinc, and vitamin B12 are essential for thyroid health, and deficiencies in any of these can exacerbate thyroid dysfunction, making it harder to manage the condition effectively. While acid blockers may alleviate acid reflux, they hinder the absorption of these crucial nutrients, leading to long-term negative impacts on thyroid health.
Magnesium is vital for over 300 biochemical processes, many supporting thyroid function. A magnesium deficiency can increase the risk of autoimmune conditions like Hashimoto’s thyroiditis, where the immune system attacks the thyroid gland, further impairing thyroid function and hormone balance.
Iron is another critical mineral for thyroid hormone production. Without sufficient iron, the body struggles to produce enough thyroid hormones, contributing to hypothyroidism. Similarly, vitamin B12 plays a key role in energy and cognitive function. Those with thyroid conditions, such as Hashimoto’s disease, often have low B12 levels, and acid blockers can reduce its absorption, leading to symptoms like fatigue, cognitive decline, and mood swings.
Maintaining adequate magnesium, iron, zinc, and B12 levels is crucial for individuals with thyroid conditions to avoid worsening symptoms and increasing complications. A careful evaluation of acid blocker use is essential to prevent further nutrient depletion, and consulting with a healthcare provider can help explore alternative treatments and protect thyroid health.
3. Acid Blockers and Hypothyroidism
For individuals with hypothyroidism, acid blockers can present significant challenges in managing their thyroid condition. These medications, including Levothyroxine (branded as Synthroid) and Natural Desiccated Thyroid (NDT), are crucial for maintaining adequate thyroid hormone levels. However, acid blockers reduce stomach acid production, which impairs the body’s ability to absorb and utilize these medications effectively. As a result, patients may experience worsened hypothyroid symptoms, such as fatigue, weight gain, and hair loss.
One major concern with acid blockers and hypothyroidism is that reduced absorption of thyroid medications isn’t just about the timing of their administration. Even if thyroid medications are taken hours apart from acid blockers, the ongoing reduction in stomach acid throughout the day can still reduce the effectiveness of these medications. This can make it more difficult for individuals to maintain stable thyroid hormone levels, potentially leading to frequent adjustments in medication dosages and fluctuations in thyroid function.
For people with hypothyroidism, maintaining stable thyroid hormone levels is essential for managing symptoms and overall health. Given the negative impact of acid blockers on medication absorption, individuals with hypothyroidism should carefully evaluate their use of these drugs.
Alternative treatments for managing acid reflux, such as dietary changes or natural remedies, may offer better solutions without affecting thyroid health. Consulting a healthcare provider to explore other options for managing acid reflux can help improve digestive and thyroid health.
4. Acid Blockers Raise SIBO and Dysbiosis Risk
Acid blockers significantly increase the risk of small intestinal bacterial overgrowth (SIBO) and gut dysbiosis by altering the balance of bacteria in the gut. The microbiome, a diverse community of bacteria in the digestive tract, plays an essential role in maintaining overall health, regulating immune function, controlling appetite, and managing inflammation. However, when acid production is reduced due to acid blocker use, it creates an environment that encourages harmful bacteria to grow, potentially leading to infections and digestive issues.
One of the key risks associated with acid blockers is their role in promoting SIBO, a condition where harmful bacteria overgrow in the small intestine. This bacterial imbalance can cause a range of digestive symptoms, including bloating, gas, constipation, diarrhea, and abdominal discomfort. Over time, SIBO can lead to chronic inflammation and poor nutrient absorption, contributing to further health issues.
Dysbiosis, an imbalance between beneficial and harmful bacteria in the gut, is another potential consequence of long-term acid blocker use. The low-acid environment created by acid blockers allows harmful bacteria like Clostridium difficile to thrive, increasing the risk of infection. Discontinuing acid blockers can help the gut microbiome recover, although the process may take time.
In addition to stopping medication, probiotics and prebiotics may be necessary to restore gut bacteria balance. This helps prevent complications like inflammation and nutrient deficiencies, ensuring better gut health and overall well-being.
5. Inflammation from Acid Blockers and Thyroid Impact
Acid blockers effectively reduce acid reflux symptoms but can also contribute to gut inflammation, which affects thyroid function. The gut converts thyroid hormone T4 into its active form, T3, needed to regulate metabolism and energy levels. Gut inflammation from SIBO, dysbiosis, or prolonged acid blocker use can impair this conversion process, leading to lower levels of active thyroid hormone in the body.
For individuals with thyroid conditions, particularly hypothyroidism, gut inflammation can worsen symptoms by reducing free thyroid hormone levels. The gut is critical in maintaining hormone balance, and inflammation disrupts this delicate equilibrium. Chronic inflammation complicates thyroid health by promoting autoimmune responses, exacerbating conditions like Hashimoto’s thyroiditis. In Hashimoto’s, the immune system attacks the thyroid gland, leading to further thyroid dysfunction. Addressing gut inflammation may indirectly improve thyroid function by supporting better hormone conversion and reducing immune attacks.
Reducing inflammation can occur through dietary changes, such as increasing anti-inflammatory foods and avoiding processed foods. In some cases, stopping the use of acid blockers may also help reduce inflammation and restore normal thyroid function. For thyroid patients, managing gut health is essential to ensure proper thyroid function and prevent additional complications from arising.
What Causes Acid Reflux and GERD?
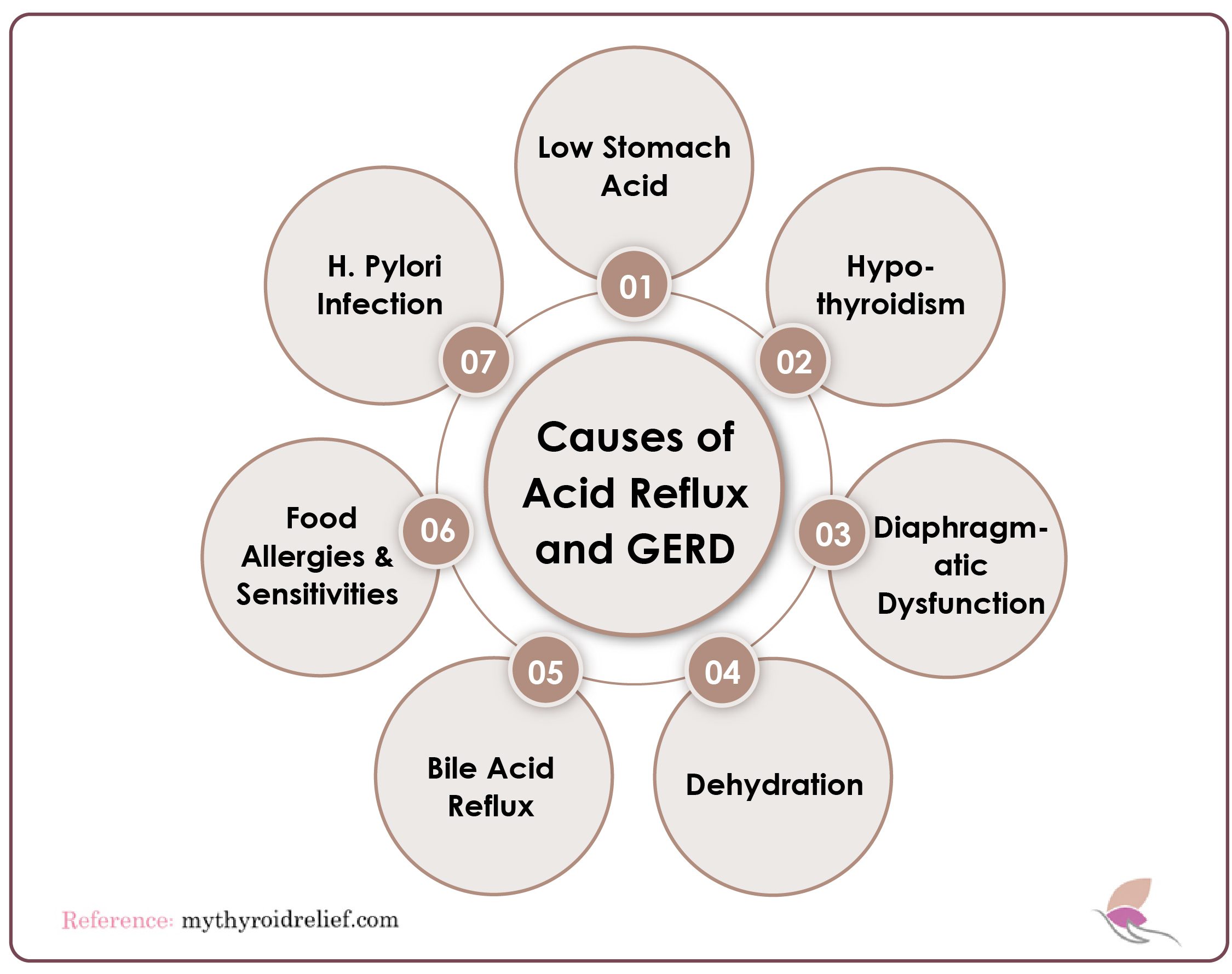
When diagnosing acid reflux or GERD, doctors consider various underlying causes. GERD is often a symptom of other health issues, meaning multiple factors may contribute to its development. Understanding the root causes of GERD is crucial for finding effective treatment.
1. Low Stomach Acid and Acid Blockers
Stomach acid is essential for absorbing nutrients, but many mistakenly believe that GERD is caused by excessive stomach acid. In reality, high stomach acid is rarely found in those with GERD. Some individuals have experienced relief by taking apple cider vinegar or hydrochloric acid supplements. If low stomach acid is part of the problem, adding acid (rather than reducing it) may help relieve GERD symptoms.
2. H. Pylori Infection and Acid Reflux
Helicobacter pylori is a bacterium that causes stomach inflammation and reduces acid production, which can contribute to GERD, ulcers, and even stomach cancer. This infection spreads through close contact, such as kissing or sharing utensils. Although some people show no symptoms, others may experience burping, bloating, heartburn, nausea, and stomach pain. Treating an H. pylori infection is essential for resolving these symptoms and preventing further complications.
3. Food Allergies and Stomach Reflux
Food intolerances, particularly gluten, have been shown to trigger GERD symptoms. Studies link celiac disease and non-celiac gluten intolerance to GERD, with many finding relief by eliminating gluten from their diet.
4. Bile Acid Reflux
Bile acid reflux occurs when bile from the small intestine backs up into the stomach. It is more common in individuals without a gallbladder. Similar to GERD, bile acid reflux is linked to dysfunction in the pyloric valve and can be worsened by low stomach acid, stress, or an H. pylori infection.
5. Dehydration and Acid Reflux
Proper hydration is essential for digestion. Dehydration can impair the body’s ability to produce stomach acid, bile, and bicarbonate, all of which are necessary for digestion.
6. Diaphragmatic Dysfunction and Acid Reflux
Diaphragmatic dysfunction can affect the lower esophageal sphincter (LES), allowing stomach acid to flow back into the esophagus and causing acid reflux. While acid blockers can help manage symptoms, they don’t address the underlying dysfunction.
7. Hypothyroidism as a Potential Cause of Acid Reflux and GERD
Hypothyroidism, a condition where the body produces insufficient thyroid hormones, can weaken the LES, leading to acid reflux and GERD. By addressing thyroid imbalances with therapies like T3 hormone treatment, you can potentially improve digestion, increase stomach acid production, and reduce GERD symptoms.
Alternative Approaches to Managing Acid Reflux and GERD
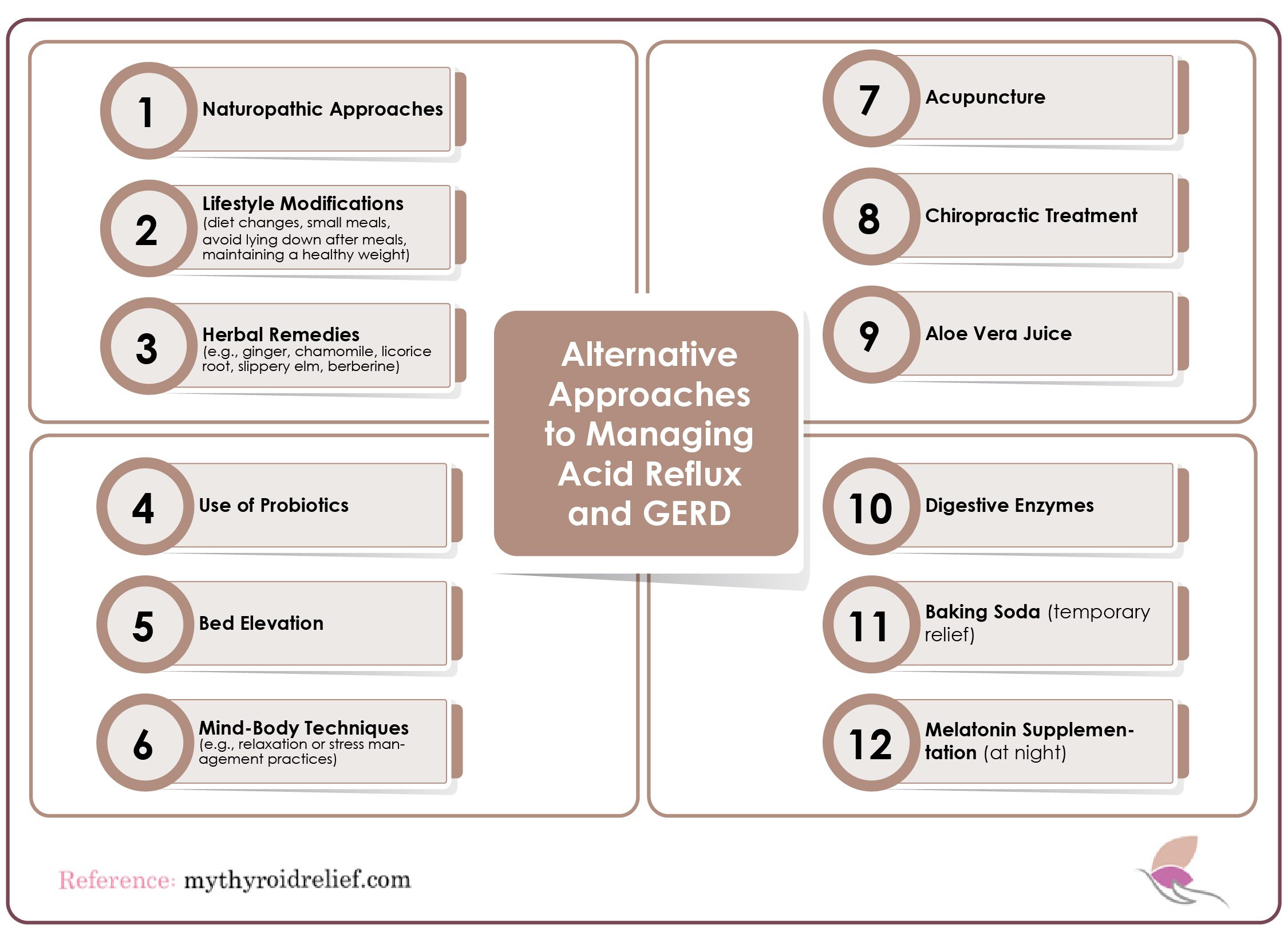
1. Naturopathic Approaches
Naturopathic medicine emphasizes treating the root causes of gastroesophageal reflux disease (GERD) rather than merely alleviating symptoms. By focusing on strengthening the lower esophageal sphincter (LES), balancing stomach acid levels, and promoting the healing of irritated tissues, naturopathic methods can provide long-term relief.
This holistic approach may include dietary changes, lifestyle modifications, and the use of herbal remedies tailored to the individual’s needs. By restoring balance within the body, these treatments can potentially reduce reliance on conventional acid blockers, which often come with side effects.
Consulting with a qualified naturopathic practitioner can help create a personalized plan that addresses the specific underlying causes of GERD.
2. Lifestyle Modifications for GERD Relief
Implementing simple lifestyle modifications can make a significant difference in managing GERD symptoms. One effective change is to identify and avoid trigger foods, which commonly include spicy dishes, citrus fruits, and high-fat meals. Additionally, consuming smaller meals throughout the day can alleviate pressure on the LES and reduce the likelihood of acid reflux. Avoid lying down immediately after eating; wait at least two to three hours before reclining. Finally, maintaining a healthy weight is crucial, as excess weight can place additional strain on the LES, worsening GERD symptoms.
3. Herbal Remedies
Certain herbs traditionally soothe digestion and ease GERD symptoms. Chamomile’s anti-inflammatory properties calm the stomach, aiding digestion. Ginger helps digestion, reduces nausea, and benefits reflux sufferers. Licorice root protects the stomach lining, soothing irritation. Slippery elm’s mucilage coats the esophagus, providing relief. Incorporating these herbs into your diet, whether through teas or supplements, may help manage GERD symptoms effectively.
4. Probiotics and GERD
Probiotics are vital for maintaining gut health and can benefit individuals suffering from GERD and hypothyroidism. These beneficial bacteria help restore the gut microbiome’s natural balance, which is often disrupted by acid blockers and poor dietary habits. Probiotic supplements or fermented foods such as kefir, yogurt, and kombucha are excellent sources of these health-promoting bacteria. Regularly consuming probiotics may help reduce inflammation and improve overall digestion, potentially leading to a decrease in GERD symptoms. Additionally, a healthy gut environment can enhance nutrient absorption, which is crucial for individuals managing thyroid conditions.
5. Bed Elevation for GERD
Elevating the head of your bed is a simple yet effective method to prevent nighttime acid reflux. By using bed risers or a wedge pillow, you can create an incline that allows gravity to keep stomach acid from flowing back into the esophagus while you sleep. This position can significantly reduce nighttime symptoms and improve sleep quality, which is essential for overall health. It’s advisable to elevate the head by at least six to eight inches for optimal results. Consistently using this method can lead to fewer awakenings due to discomfort and a more restful night’s sleep.
6. Mind-Body Techniques
Managing stress and anxiety is crucial for individuals with GERD, as these emotions can exacerbate symptoms. Mind-body techniques, including yoga, meditation, and deep breathing exercises, can effectively promote relaxation and reduce stress levels. Practicing these techniques regularly can help soothe the nervous system and may even improve digestive function. For instance, yoga combines gentle physical movement with breath control, which can help stimulate digestion and reduce tension in the abdomen. Incorporating mind-body practices into your daily routine can contribute to better overall management of GERD symptoms.
7. Acupuncture
Emerging research suggests that acupuncture may be an effective treatment for reducing GERD symptoms by regulating stomach acid levels and enhancing the function of the lower esophageal sphincter (LES). This traditional Chinese medicine technique involves inserting fine needles into specific points on the body to promote healing and balance. Studies have indicated that acupuncture can improve LES pressure, potentially reducing instances of acid reflux. Electroacupuncture (EA), a variation that uses electrical stimulation, may further enhance these benefits. Consulting a licensed acupuncturist can help determine an appropriate treatment plan tailored to individual needs.
8. Chiropractic Care
Chiropractic adjustments may provide relief for individuals suffering from GERD by improving nerve function related to digestion. Misalignments in the spine can disrupt nerve signals that control the digestive system, potentially exacerbating GERD symptoms. By correcting these misalignments, chiropractors aim to restore proper nerve function, which may help regulate digestive processes and improve overall gastrointestinal health. Additionally, chiropractic care can promote relaxation and alleviate tension, further benefiting individuals dealing with the discomfort of acid reflux. Regular chiropractic sessions can be a valuable addition to a comprehensive GERD management plan.
9. Aloe Vera Juice
Aloe vera juice is well-known for its soothing properties and may help reduce inflammation in the esophagus caused by GERD. Consuming aloe vera juice can provide a cooling effect, helping to calm irritation and promote healing of the esophageal lining. People often use this natural remedy to relieve heartburn and acid reflux, making it a popular alternative treatment. It’s important to choose a high-quality, organic aloe vera juice free from added sugars and artificial ingredients. Incorporating aloe vera juice into your daily routine may contribute to improved digestive health and relief from GERD symptoms.
10. Digestive Enzymes
Taking digestive enzyme supplements can significantly help those struggling with GERD by aiding in the breakdown of food and reducing acid reflux symptoms. These enzymes facilitate digestion by breaking down carbohydrates, fats, and proteins, which can alleviate the burden on the stomach. When food is properly digested, it is less likely to ferment and produce excess gas, which can contribute to reflux. Incorporating digestive enzymes into your diet may also promote a more efficient digestive process, enhancing nutrient absorption. Consulting a healthcare professional can help determine the appropriate enzyme blend for individual needs.
11. Baking Soda
Baking soda is a common household remedy that can provide temporary relief from heartburn and acid reflux. Mixing a small amount of baking soda with water can help neutralize stomach acid, offering quick relief from discomfort. However, it’s important to use this remedy sparingly, as excessive consumption can lead to other digestive issues, such as bloating and gas. Use baking soda only as an occasional quick fix for GERD symptoms, not as a long-term management solution. Always consult a healthcare professional if you experience frequent acid reflux to determine a more comprehensive management plan.
12. Melatonin
Melatonin, a hormone primarily known for regulating sleep, may also have gastroprotective properties that help alleviate nighttime acid reflux. Some studies suggest melatonin may improve esophageal motility and enhance the mucosal barrier, reducing GERD symptoms. A 2010 study showed that combining melatonin with omeprazole could shorten treatment duration and lessen side effects. Melatonin can effectively complement a GERD management plan, but consulting a healthcare provider for dosage is essential. Integrating melatonin into your routine may promote better sleep quality while addressing reflux symptoms.
Why Consider Alternative Approaches?
As awareness of the risks associated with long-term acid blocker use grows, many individuals are turning to alternative approaches for managing acid reflux and related digestive issues. Research has raised significant concerns about ranitidine (Zantac), linking it to cancer risks due to the contaminant NDMA.
This has led to a reevaluation of the safety of these medications, alarming both healthcare professionals and patients. Proton pump inhibitors (PPIs), widely prescribed acid blockers, are associated with memory loss, weakened bones, and an increased risk of pneumonia. Memory loss is particularly concerning because it can impair cognitive function and diminish quality of life. The impact on bone health is equally alarming, as long-term PPI use is linked to a higher risk of osteoporosis and fractures.
Additionally, the suppression of stomach acid can compromise the body’s natural defense against pathogens, leading to an increased susceptibility to infections. Given these risks, individuals may benefit from exploring alternative approaches to managing acid reflux symptoms.
Lifestyle changes, such as dietary modifications and weight management, can significantly improve symptoms. Stress reduction techniques such as avoiding trigger foods, practicing mindful eating, and engaging in regular physical activity can also alleviate symptoms naturally, without the risks of medication. By considering these alternatives, individuals can take control of their digestive health while minimizing the risks of long-term medication use.
Conclusion
While acid blockers can alleviate GERD symptoms, they may also have unintended effects on thyroid health and digestion. Conditions like diaphragmatic dysfunction, H. pylori infection, or hypothyroidism may contribute to GERD. A holistic approach to GERD management—incorporating lifestyle changes, natural remedies, and addressing underlying thyroid issues—can lead to better symptom control and overall health. Always consult a healthcare professional before making any changes to your treatment plan.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2784889
- https://www.healthline.com/health/gerd/thyroid
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5751186
- https://link.springer.com/10.1007/978-3-319-45013-1_27
- https://www.bswhealth.com/blog/16-things-that-can-mess-with-your-thyroid-health-and-medication