Table of Contents
Toggle
Introduction
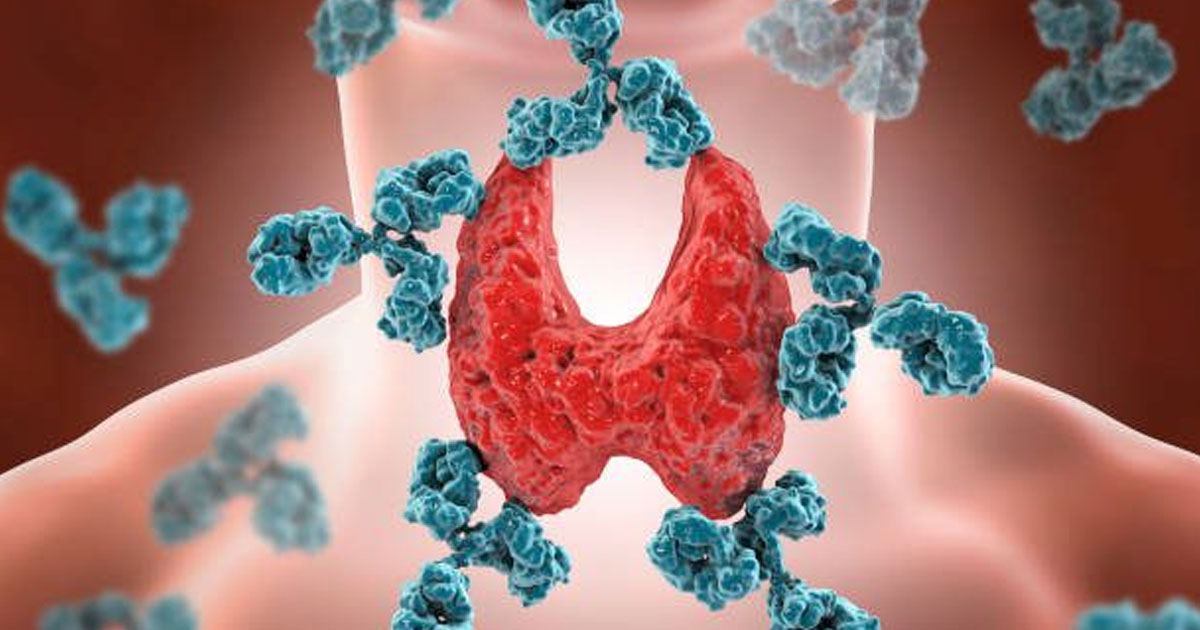
Did you know that the majority of thyroid diseases involve an autoimmune element? (1) Hashimoto’s thyroiditis, for instance, is an autoimmune disorder that targets the thyroid gland. In this condition, the immune system mistakenly identifies the thyroid as a threat and begins attacking it, leading to the gradual destruction of the gland.
Additionally, if the destruction of the thyroid tissue continues for a long time, the gland will be unable to produce thyroid hormone. In this case, the immune system will produce antibodies that erroneously target thyroid cells, treating them as foreign invaders like bacteria or viruses. Consequently, the immune response damages the cells of the thyroid, resulting in hypothyroidism.
Most cases of Hashimoto’s thyroiditis are discovered after the condition has progressed to the very advanced stages, where the thyroid gland has undergone significant damage. In this article, I’d like to discuss Hashimoto thyroiditis extensively and how it can cause an underactive thyroid.
An Overview of Hashimoto thyroiditis
Hashimoto’s thyroiditis is an autoimmune condition of the thyroid (3) that targets and attacks the thyroid gland. This illness is characterized by antibodies circulating in the bloodstream that bind to specific components of the thyroid gland, causing inflammation.
Moreover, the immune system recognizes certain parts of the thyroid as foreign and begins to attack the thyroid tissue over time, mistaking it for harmful viruses or bacteria. Regrettably, many conventional doctors and healthcare providers focus solely on thyroid hormone levels such as TSH, T3, and T4, neglecting to test for thyroid antibodies. This narrow focus makes it harder to fully assess and treat Hashimoto’s thyroiditis, making it more difficult to stop the thyroid gland’s damage before it becomes irreversible.
Furthermore, it’s crucial for healthcare providers to test additional thyroid hormones like FT4, FT3, RT3, TSH, and T4, as well as antibodies such as Thyroid Peroxidase Antibodies (TPOAb), Thyroglobulin Antibodies (TgAb), and Thyroid Stimulating Immunoglobulin (TSI), to rule out Hashimoto’s or Grave diseases.
Additionally, diagnosing Hashimoto’s thyroiditis requires understanding its underlying causes and how the condition manifests itself. By recognizing these factors, healthcare providers can effectively manage the disease’s symptoms and provide appropriate treatment.
Symptoms of Hashimoto's disease
Furthermore, Hashimoto’s thyroiditis typically develops gradually, progressing slowly over several years. Initially, individuals may not experience noticeable signs of the illness. The symptoms of this disease can vary significantly among individuals. Due to the overlap of symptoms with other conditions, consulting a certified functional healthcare provider is crucial for accurate diagnosis and effective treatment. Their approach can help identify the root cause of the illness.
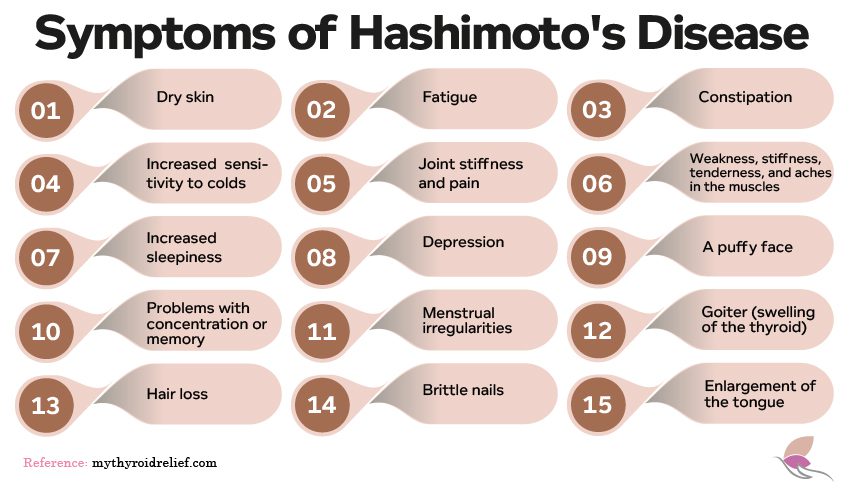
This list is the typical symptoms associated with Hashimoto’s disease:
- Dry skin
- Sluggishness fatigue
- Constipation
- Increased sensitivity to cold
- Muscle weakness
- Joint stiffness and pain
- Stiffness, tenderness, and aches in the muscle
- Increased sleepiness
- Depression
- A puffy face
- Problems with concentration or memory
- Excessive or irregular menstrual bleeding
- Goiter (swelling of the thyroid)
- Hair loss
- Brittle nails
- Enlargement of the tongue
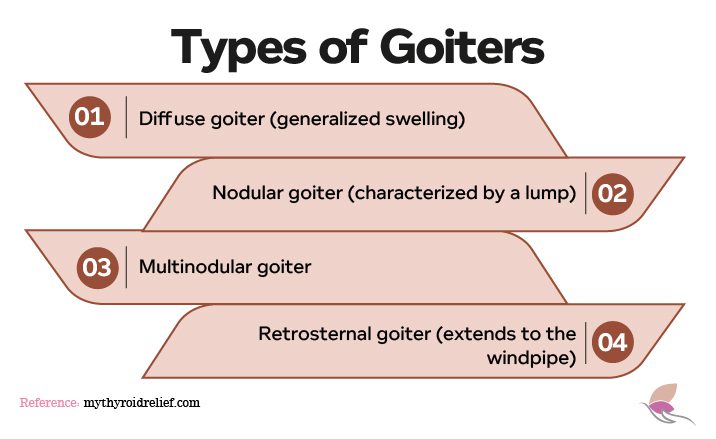
Moreover, Hashimoto’s thyroiditis can cause the development of goiters, which are enlarged thyroid glands. These goiters can lead to visible swelling in the neck and may cause symptoms such as difficulty swallowing or breathing.
There are four main types of goiters:
- Diffuse goiter, featuring a smooth and generalized swelling, involves uniform enlargement of the entire thyroid gland,
- Nodular goiter is characterized by one or more nodules within the thyroid tissue
- Multinodular goiter is characterized by multiple nodules scattered throughout the thyroid gland.
- Retrosternal goiter is located behind the sternum or breastbone.
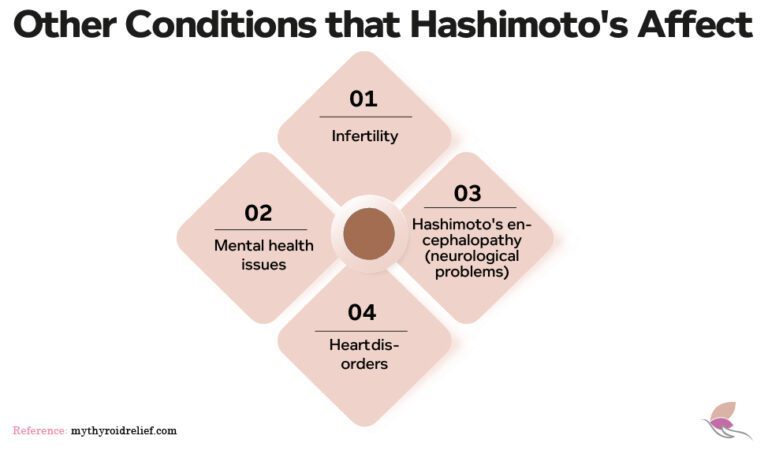
Furthermore, Hashimoto’s Thyroiditis Can Also Affect Other Organs and Systems in the Body:
Hashimoto’s thyroiditis can cause changes in heart rate and rhythm, increasing the risk of cardiovascular issues such as heart disease and hypertension.
Disruptions caused by Hashimoto’s can result in symptoms like fatigue, depression, memory problems, and difficulty concentrating.
Hashimoto’s can affect menstrual regularity and fertility in women, potentially resulting in complications such as miscarriage, preterm birth, and preeclampsia for pregnant women.
Hashimoto’s can contribute to muscle weakness, joint pain, and stiffness, making daily activities more challenging.
Some people with Hashimoto’s may experience digestive issues like constipation, bloating, and abdominal discomfort.
Changes in thyroid hormone levels due to Hashimoto’s can result in skin dryness, itching, and changes in texture.
Hashimoto’s thyroiditis can slow down metabolism, leading to weight gain and difficulty losing weight despite maintaining a healthy diet and exercise routine.
Hashimoto’s can disrupt the balance of hormones produced by the thyroid gland, leading to secondary hormonal imbalances affecting energy levels, mood, and metabolism.
In addition, other underlying conditions may also trigger this autoimmune disease, like infertility, mental health issues, heart disorders, and neurological problems.
Hashimoto’s Thyroiditis extends its impact beyond thyroid function, influencing various aspects of health and well-being, including fertility, hormonal balance, cardiovascular health, sexual function, and neurological well-being.Hashimoto’s Thyroiditis extends its impact beyond thyroid function, influencing various aspects of health and well-being, including fertility, hormonal balance, cardiovascular health, sexual function, and neurological well-being.
1. Infertility
Women with Hashimoto’s thyroiditis often face challenges related to fertility, including difficulties conceiving and an increased risk of miscarriages. Additionally, there’s a heightened possibility of congenital disabilities in children born to these women.
- Role of Hormones in Autoimmune Conditions:
Estrogen is believed to play a significant role in the development of autoimmune thyroid disorders like Hashimoto’s. Furthermore, hormonal shifts during critical life stages such as pregnancy, puberty, and perimenopause can trigger or exacerbate the condition. Estrogen fluctuations can also influence the body’s thyroid hormone requirements, especially when nutrient deficiencies are present, potentially causing autoimmune thyroid issues.
- Impact of Prolactin and Testosterone:
Besides estrogen, prolactin and testosterone also influence the immune system and can affect autoimmune diseases like Hashimoto’s thyroiditis. In female patients, elevated prolactin levels—typically associated with breastfeeding—may occur even in non-breastfeeding Hashimoto’s patients, potentially impacting fertility and thyroid antibody levels. Additionally, testosterone, known for its immune-modulating properties, can also affect autoimmune conditions. Low levels of testosterone have been associated with an increased risk of autoimmune diseases, which can exacerbate the symptoms and progression of Hashimoto’s thyroiditis by influencing the body’s inflammatory response.
- Sexual Dysfunction in Thyroid Patients:
Thyroid disorders often result in sexual dysfunction for both men and women, with studies showing a high prevalence of low libido. Men with hypothyroidism commonly experience sexual issues, including erectile dysfunction, reduced libido, delayed ejaculation, and sperm abnormalities, all of which can affect overall sexual health and fertility. Furthermore, hyperthyroidism also leads to low semen motility, density, and volume.
2. Heart Disorders
Mild hypothyroidism can have a significant impact on heart health (13). For instance, it can lead to an increase in low-density lipoprotein cholesterol due to thyroid hormone dysregulation, which in turn can cause the hardening of arteries and elevate the risk of stroke and heart attacks.
While most cases of hypothyroidism are mild, severe cases can result in a condition called pericardial tamponade, where the heart is unable to pump enough blood, leading to a drastic reduction in blood pressure.
This complication is characterized by brain swelling and profound, debilitating neurological symptoms, known as Hashimoto’s encephalopathy. This rare condition affects about two out of every 100,000 people annually, typically between the ages of 41 and 44 (14). It is worth noting that females have a prevalence four times higher than males.
3. Hashimoto's Encephalopathy
Hashimoto’s Encephalopathy is a rare neurological complication associated with Hashimoto’s Thyroiditis. It involves autoimmune-mediated inflammation of the brain, leading to various neurological symptoms like cognitive impairment, seizures, and psychiatric manifestations.
Treatment typically includes corticosteroids to suppress the autoimmune response and immunosuppressive agents in refractory cases. Prompt recognition and management are crucial to prevent irreversible neurological damage.
Furthermore, this condition highlights the systemic nature of autoimmune thyroid diseases, emphasizing the need for comprehensive evaluation and management of associated neurological complications.
Missing the Diagnosis of Hashimoto Thyroiditis
Moreover, , diagnosing Hashimoto’s thyroiditis is crucial because understanding that you have this disease changes your approach to treatment. While doctors often use thyroid hormone replacement to address regular hypothyroidism, most Hashimoto patients may require thyroid medication at some point in their lives.
Early intervention can delay or even reverse the progression of the disease, avoiding long-term destruction and the lifelong need for thyroid medication. To accomplish this, it’s essential first to determine if you have Hashimoto’s thyroiditis.
Why does this matter? Because most doctors only assess the function of the thyroid gland and offer treatment when the gland has been significantly compromised, leading to symptoms like fatigue, hair loss, cold intolerance, and weight gain.
It’s important to note that many doctors do not consider diagnosing Hashimoto’s as helpful or necessary because it doesn’t change their treatment plan.
Conventional doctors often take a “wait and see” approach (5), allowing the thyroid gland to be continually attacked and destroyed until the patient eventually requires thyroid medication. However, if this resonates with your situation, know you are not alone!
Root Causes of Developing Hashimoto Thyroiditis
Furthermore, researchers and medical doctors have long believed that autoimmune diseases have no cure and that administering levothyroxine is the only solution. However, early management of inflammation, addressing potential dietary considerations, and exploring other individualized treatment options can significantly delay or even reverse the progression of the disease. Additionally, while we don’t have all the answers yet, several factors can contribute to the onset of this illness.
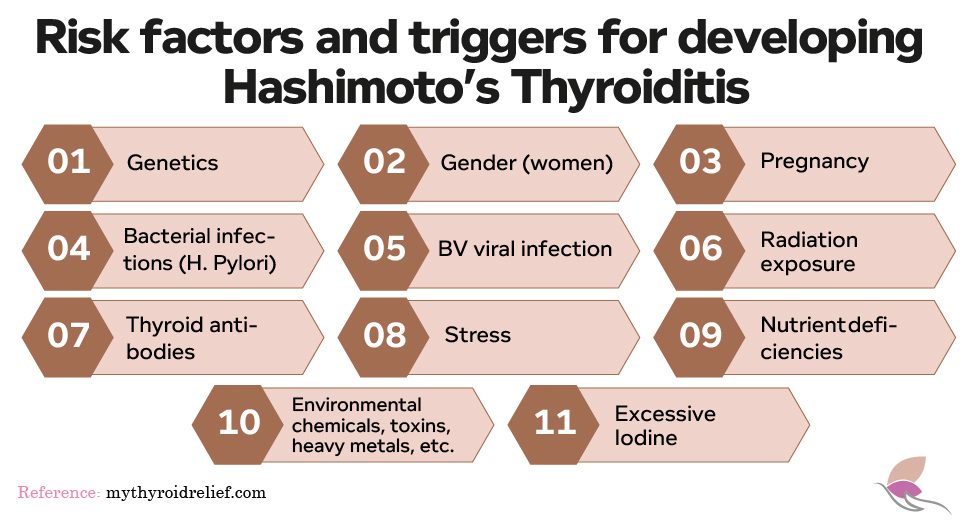
- Genetics
Several inherited genes are associated with Hashimoto’s disease. The most common are HLA-DR3 and HLA-DR5, which are usually found in Caucasians race. Having one of these genes does not mean you will develop Hashimoto’s disease; it only means that your risk is higher (21).
Relatives of people with Hashimoto’s disease also have a higher risk of developing the disease. And because it’s more common in women, female relatives have the highest risk.
First-degree relatives, especially children, have a higher incidence—up to nine times—of having the condition (22). There is also a greater incidence of Hashimoto’s in twins than in the general population (23).
- Gender
Women are more likely to develop Hashimoto’s disease than men, and researchers believe this may be because their sex hormones, estrogen and progesterone (24), might play a role in making them more prone to Hashimoto’s. Additionally, some women may have thyroid issues in the first year after giving birth, but these usually go away on their own. However, they can sometimes lead to a diagnosis of Hashimoto’s later in life.
- Bacterial infections
Autoimmune diseases, including Hashimoto’s, may be set off by numerous fungal, parasitic, and yeast infections in the gastrointestinal system. People who carry these types of stomach bacteria don’t always show symptoms. However, there is not enough detailed research to ascertain how particular bacterial infections cause autoimmune thyroid conditions or how to lower their risks (25).
Research suggests that autoimmune diseases, such as Hashimoto’s, could be triggered by various fungal, parasitic, yeast, and candida infections within the gastrointestinal system. Interestingly, individuals harboring these types of stomach bacteria may not always display symptoms. However, despite this correlation, there is a lack of comprehensive research elucidating the precise mechanisms through which specific bacterial infections contribute to autoimmune thyroid conditions (25).
- Radiation exposure
A correlation between exposure to radiation and developing Hashimoto’s disease has been found. The illness is prevalent in cancer patients undergoing radiation treatment and those subjected to nuclear fallout (26).
- Thyroid antibodies
They are typical in individuals with Hashimoto’s disease. Antibodies associated with this condition are frequently present for years before a diagnosis of Hashimoto’s disease is made. Test results may indicate that levels are normal. However, they indicate that the thyroid can no longer generate enough hormones.
While most people with Hashimoto’s disease have particular antibodies, about 5% do not. People with no antibodies tend to suffer from a milder form of the illness.
Potential Triggers of Hashimoto's.
Additionally, let’s explore Hashimoto’s potential triggers to gain a deeper understanding.
1. Stress
Stress is recognized as a significant factor that can exacerbate symptoms and contribute to the development or worsening of Hashimoto’s thyroiditis. However, it’s important to understand that Hashimoto’s is a complex autoimmune condition with multiple underlying factors, and stress is just one piece of a complex illness.
Another key point is that while significant life events and chronic stressors can impact health and trigger autoimmune conditions like Hashimoto’s thyroiditis, there are other factors such as genetic predisposition, hormonal imbalances, and environmental triggers also play a role.
Therefore, while eliminating stress may not be possible, we can take steps to better manage and cope with it. Adopting healthy coping mechanisms such as meditation, regular exercise, adequate sleep, and seeking support from friends, family, or a therapist can help mitigate the effects of stress on our health and well-being.
- EBV viral infection
The Epstein-Barr virus (EBV) is also part of the herpes virus family and is linked to Hashimoto’s thyroiditis. As a result, the Epstein-Barr virus (EBV) persists in the body for life, entering a dormant state. During this time, the virus remains inactive but can reactivate under certain conditions, such as stress, weakened immunity, hormonal fluctuations, or immunosuppressants. However, when reactivated, EBV can cause symptoms to resurface and worsen Hashimoto’s symptoms by affecting the immune system.
3. Helicobacter pylori
This bacteria is commonly found in the stomach and is infamous for its association with stomach ulcers. However, its impact extends beyond gastrointestinal issues, as it also disrupts the immune system, contributing to the development of Hashimoto’s thyroiditis and potentially triggering flare-ups in treated patients.
Research indicates that over 50 percent of the global population has been infected with H. pylori. Furthermore, therapies and medications that reduce stomach acid levels can heighten the risk of H. pylori infection.
- Nutrient deficiencies
Nutrients play an essential role in the body’s functions. In some instances, deficiencies in vitamins D and B12 and the minerals zinc, magnesium, selenium, and Iodine can reduce symptoms or flare-ups in Hashimoto’s disease.
For example, Vitamin D deficiency can weaken your immune system (8), increasing your susceptibility to infections and stress.
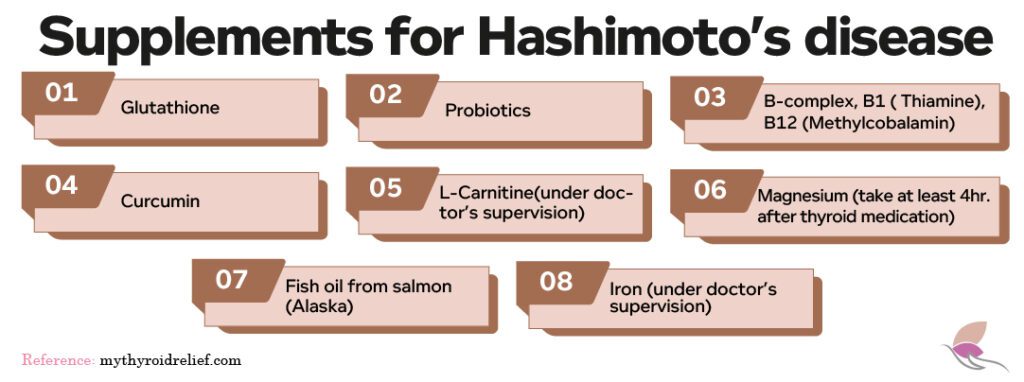
Other essential nutrients for your thyroid include:
- Glutathione
- Probiotics
- B-complex, B1 ( Thiamine), B12 (Methylcobalamin)
- Curcumin
- L-Carnitine
- Magnesium (taken at least 4 hours after thyroid medication)
- Fish oil from salmon (Alaska)
- Iron
In addition, supplements such as alpha-lipoic acid and N-acetyl cysteine may benefit individuals with Hashimoto’s thyroiditis. Every person with Hashimoto’s should undergo testing for nutrient deficiencies to manage this condition. A doctor should prescribe the appropriate dosages and regularly retest to ensure the levels are within a healthy range.
It’s important to be aware that excessive levels of these vitamins and supplements can have negative health consequences. Additionally, taking periodic breaks from these supplements is crucial to prevent an increase in IGF-1 (growth hormone) levels. Prolonged use of vitamins and supplements can disrupt hormonal balance and lead to adverse health effects. Therefore, it’s essential to resume supplementation when necessary, under medical supervision.
- Bacterial/fungal overgrowth syndromes (SIBO & SIFO)
Bacterial and fungal overgrowth syndromes, known as SIBO and SIFO, highlight the importance of gut health. It is important to realize that your gut is a crucial focal point for immune system regulation and a barrier between your body and the external environment.
SIBO, or small intestinal bacterial overgrowth, and SIFO, or small intestinal fungal overgrowth, occur when there’s an imbalance in the gut microbiota. Usually, your gut harbors various types of bacteria that play essential roles in nutrient absorption and hormone regulation. However, lifestyle factors such as diet and stress can disrupt this delicate balance, creating an environment conducive to the overgrowth of certain bacterial and fungal species.
- Pain in the stomach, especially after eating
- Diarrhea
- Bloating
- Cramps
- Indigestion
- Gas
- A regular feeling of fulness
This problem tends to be exaggerated in patients with thyroid conditions because intestinal motility slows down during low thyroid conditions. Your risk of SIBO increases as your intestines’ speed slows down (9). In that case, you can always test for these conditions and treat them appropriately.
Treating and restoring your gut flora will significantly improve Hashimoto’s and your overall health. However, conventional doctors may not be familiar with these overgrowth syndromes, so you may need to consult an integrative or naturopathic (holistic) doctor for tests and treatment.
- Environmental factors
Toxins and heavy metals in our food, everyday products for personal hygiene and household items, dental work, exposure to swimming pools and hot tops treated with chemicals, creams, makeup products, and perfumes can damage the thyroid and provoke an autoimmune disease.

What is the Link Between Hypothyroidism and Hashimoto's Disease?
However it is well known that Hashimoto causes hypothyroidism, but not everyone with hypothyroidism has Hashimoto’s disease.
Hypothyroidism typically results from reduced thyroid hormone production by the thyroid gland. While Hashimoto’s disease can cause hypothyroidism, other factors can contribute, like the body’s resistance to thyroid hormone, iodine deficiency, thyroid surgery or radioiodine therapy, certain medications, pituitary disorders, genetic factors, and thyroid gland inflammation can also contribute to this condition.
Whenever your thyroid gland cannot produce adequate thyroid hormone for your cells and body, you’ll have the symptoms of hypothyroidism. Most importantly, common symptoms of hypothyroidism can include weight gain, fatigue, hair loss, constipation, cold intolerance, and other issues.
Hashimoto’s disease can lead to hypothyroidism, but various factors can also play a role in disrupting thyroid hormone production. While treatments for hypothyroidism typically focus on increasing thyroid hormone levels in the body, it’s essential to address these contributing factors for comprehensive management.
The primary similarity between Hashimoto’s thyroiditis and hypothyroidism is that both conditions can co-exist in the same cases. However, some patients can have Hashimoto’s without hypothyroidism.
Laboratory Tests to Diagnose Hashimoto's
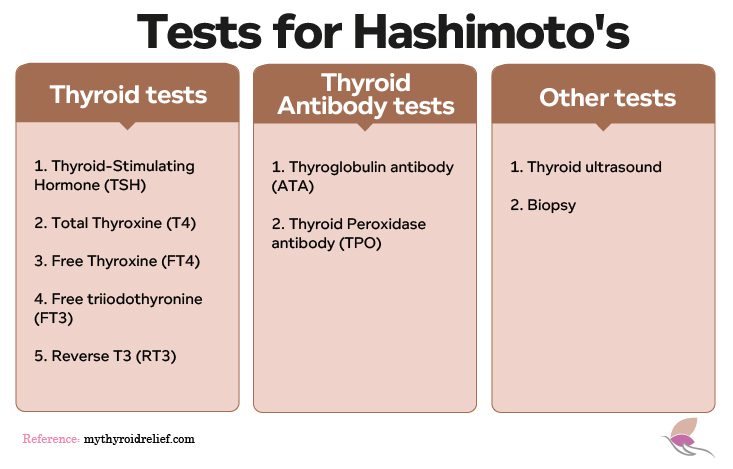
Some diagnostic tests for Hashimoto’s can be done quickly, while others may require invasive procedures.
- Thyroid tests:
- Total Thyroxine (T4)
- Free Thyroxine (T4)
- Free triiodothyronine (Free T3)
- Reverse T3Thyroid tests:
- Thyroid-stimulating hormone (TSH)
- Thyroid Antibody Tests:
- Thyroglobulin antibody
- Thyroid Peroxidase antibody
These antibody tests, like the Thyroglobulin Antibody (TGAb) and Thyroid Peroxidase Antibody (TPOAb) tests, are vital for diagnosing thyroid disorders, especially autoimmune ones like Hashimoto’s thyroiditis and Graves’ disease. To put it another way, TGAb targets thyroglobulin, a thyroid protein, while TPOAb targets thyroid peroxidase, an enzyme in hormone production. Elevated levels of these antibodies indicate autoimmune activity,
3. Thyroid ultrasound: A thyroid ultrasound is a non-invasive procedure that utilizes sound waves to create detailed images of the thyroid gland and neck lymph nodes. This imaging technique aids in diagnosing conditions like Hashimoto’s thyroiditis by detecting increased blood flow, which indicates inflammation. It can also identify pseudo nodules, artifacts produced during imaging that mimic actual nodules. Despite its effectiveness, thyroid ultrasound is simple, providing valuable insights into gland size and inflammation without invasive measures.
4. Biopsy: Though not often needed, a biopsy is crucial for diagnosing Hashimoto’s thyroiditis and other thyroid issues. A small tissue sample is taken from the thyroid gland for examination under a microscope during this procedure. The results of this analysis confirm the diagnosis and guide the decision-making process for treatment. Biopsies are typically pursued as a last resort when other tests don’t provide clear answers or when confirmation before starting treatment is necessary.
Do you know you can order your tests? Check for companies where you can order any thyroid tests if your doctor refuses to do them.
Treatment for Hashimoto's
Traditional vs. Holistic Approach
There are two main approaches to treat Hashimoto’s: traditional and holistic. Knowing about both methods is important because it helps you find the right kind of doctor for your case. It’s good to remember that regular doctors might not suggest holistic treatments, and vice versa. Let’s take a closer look at each approach:
1. Conventional Treatment for Hashimoto’s Thyroiditis
Doctors typically monitor your blood work every three months in conventional treatment for Hashimoto’s thyroiditis. At this point, they’ll wait until your thyroid stimulating hormone (TSH) reaches a certain level, indicating hypothyroidism, before diagnosing you.
Your doctor will initiate treatment with levothyroxine or Synthroid, adjusting your medication according to your TSH level. Conventional treatment primarily targets TSH levels, with less emphasis on symptoms, environmental factors, and lifestyle choices.
Additionally, some patients may opt for conventional treatment simply because they’re unaware of holistic alternatives for Hashimoto’s disease. However, if traditional treatments fail to alleviate their symptoms, they may seek out holistic medicine for an alternative approach.
Can Hashimoto’s Thyroiditis Be Reversed?
In certain cases, the answer is yes! This reversal is often achieved through an alternative or functional treatment approach, which we’ll explore next.
2. Alternative/Functional Approach
The alternative/functional approach varies depending on your physician and their expertise in treating Hashimoto’s with a holistic approach.
With this in mind, alternative treatment for Hashimoto’s thyroiditis is more effective than conventional medicine because it identifies the underlying cause(s) or factors that trigger Hashimoto’s thyroiditis and addresses them one by one.
In alternative treatment, a knowledgeable and caring integrative doctor creates a comprehensive health plan to manage these factors, which include stress, nutrient deficiency, testing for heavy metals, food allergies, environmental toxins, lack of exercise, and an unhealthy, non-organic diet.
In this case, once a patient has been diagnosed with Hashimoto’s, traditional doctors will treat you with synthetic thyroid hormone medication. However, they are not told why they have Hashimoto’s, how this autoimmune condition affects their future, and what they can do to improve their condition and support their thyroid apart from the usual medication intake.
Most clinicians often dismiss autoimmune conditions as merely the result of specific genes, failing to take them seriously. Moreover, many doctors believe that autoimmune conditions cannot be reversed.
As stated previously, some of the most important factors contributing to autoimmune conditions include genetic predisposition, external triggers, leaky gut (intestinal permeability), and exposure to chemicals, toxins, and heavy metals. Eliminating these factors can lead to remission of the autoimmune condition. This explains why targeting the underlying cause of Hashimoto’s symptoms may reverse the condition.
Alternative treatments may include the following:
- Dietary approach
When managing Hashimoto’s thyroiditis and addressing autoimmune conditions, strategic dietary changes are often recommended. While scientific research on the direct impact of specific diets on autoimmunity remains limited, many patients have experienced positive outcomes with certain dietary approaches:
- Gluten-Free Diet: Additionally, a gluten-free diet is often recommended, as there is a well-established link between celiac disease (a form of gluten sensitivity) and autoimmune disorders. Eliminating gluten will help alleviate inflammation and improve overall well-being.
- Dairy-Free Diet: Some: individuals with autoimmune conditions may benefit from eliminating dairy products, which can improve intestinal health and reduce inflammation.
- Mediterranean Diet: This diet is gaining recognition for its potential benefits in managing autoimmune conditions. Rich in fruits, vegetables, whole grains, lean proteins, and healthy fats like olive oil, this diet emphasizes anti-inflammatory foods that may help modulate immune function.
- Autoimmune Protocol (AIP) Diet: This diet targets inflammation, pain, and other symptoms associated with autoimmune diseases such as lupus, inflammatory bowel disease (IBD), celiac disease, and rheumatoid arthritis. This protocol eliminates potentially inflammatory foods like grains, legumes, dairy, processed foods, and certain fats. Many individuals report reduced symptoms and improved overall health by focusing on nutrient-dense foods and eliminating potential triggers.
The AIP diet typically includes Lean proteins such as fish, poultry, and grass-fed meats. Vegetables, especially colorful and leafy varieties, provide essential vitamins and minerals. Healthy fats like avocado, olive oil, and coconut oil. Fruits, preferably low-glycemic options.
Bone broth is rich in nutrients and believed to support gut health. Fermented foods like sauerkraut and kimchi promote healthy gut macrobiotics.
In addition to dietary protocols like the Mediterranean diet and the Autoimmune Protocol (AIP) diet, choosing high-quality foods is vital for managing autoimmune conditions like Hashimoto’s thyroiditis. It is important to consider:
- Organic Produce: Opting for organic fruits and vegetables reduces exposure to harmful chemicals and increases nutrient density.
- Grass-Fed Meats: Grass-fed meats provide higher levels of beneficial nutrients like omega-3 fatty acids and CLA, supporting immune health.
- Wild-Caught Fish and Seafood: Wild-caught varieties are rich in omega-3 fatty acids and free from contaminants found in farmed fish, aiding in reducing inflammation and autoimmune symptoms.
It’s important to understand that there’s no one-size-fits-all approach to dietary management of autoimmune conditions. Each person’s response to nutritional changes may vary, and personalized adjustments are often necessary.
Consulting with a functional nutritionist can provide valuable guidance in determining the most suitable dietary plan based on individual needs and health goals.
Through trial and error, individuals can identify the foods they have allergies or sensitivities to and what foods support their immune function and overall well-being.
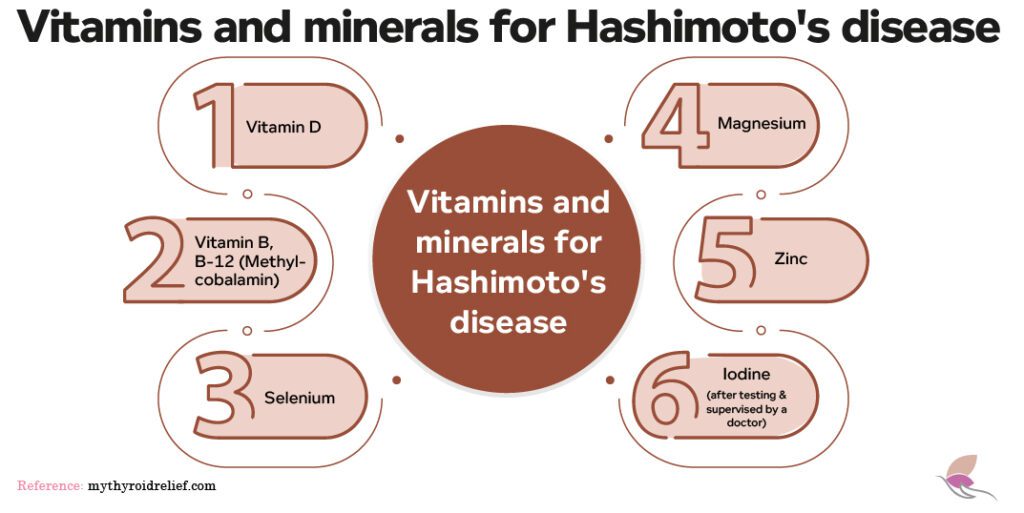
In addition, some supplements can help improve thyroid disease and boost immune function. An example is the administration of vitamin D in patients with autoimmunity. A vitamin D deficiency increases the risk of developing an autoimmune condition, including Hashimoto’s disease (17).
Other supplements, such as Selenium, Zinc, magnesium, vitamin B complex ( B-12), curcumin, iron, fish oil, probiotics, glutathione, and Iodine, may boost thyroid hormone production and peripheral thyroid conversion (18).
Like the dietary approach, your supplements should be “customized” to your needs and body. Taking supplements in excess or the wrong supplements may be counterproductive. It is important to note that some cases of Hashimoto’s may be triggered by too low or excess iodine intake.
It is recommended to test first if you have a deficiency in a particular nutrient ( vitamins and minerals) before supplementing them under the supervision of a knowledgeable functional or naturopathic doctor.
Possible Treatments for Hashimoto's disease
Moreover, Naltrexone, an FDA-approved medication primarily used for opioid withdrawal, has shown promise in managing autoimmune conditions such as Hashimoto’s disease. While the standard dose is 50mg daily, lower doses ranging from 1.5 to 4.5 mg daily have been found to modulate the immune system effectively. Studies have demonstrated its efficacy in improving cases of multiple sclerosis, Crohn’s disease, and Hashimoto’s thyroiditis.
Low-dose naltrexone enhances immune function through various mechanisms, including promoting endogenous endorphin production, DNA synthesis, and reduction of inflammation. It also slows gastrointestinal tract motility, aiding in tissue healing. By increasing T-regulatory cytokines and modulating transforming growth factor beta (TGF-β), low-dose naltrexone effectively suppresses Th-17, a group of cells that promotes autoimmunity.
Additionally, research indicates that metformin, a medication commonly used to treat type 2 diabetes, may have therapeutic effects in reversing Hashimoto’s thyroiditis. A 2021 study published in Frontiers in Cell and Developmental Biology demonstrated that metformin could reverse major immune events associated with Hashimoto’s disease. By reducing the infiltration of lymphocytes and thyroid globulin antibody (TgAb) in thyroid tissue, metformin shows promise as a potential treatment for Hashimoto’s thyroiditis.(20)
Conclusion
Understanding Hashimoto’s thyroiditis, especially after a recent diagnosis, can feel overwhelming. This autoimmune condition targets the thyroid gland, leading to various symptoms and impacting its function. However, by exploring the underlying factors of the disease and learning about available treatment options, individuals can better navigate their journey toward managing Hashimoto’s.
Taking a holistic approach to treating Hashimoto’s thyroiditis is crucial. This includes undergoing comprehensive blood work and medical tests to uncover contributing issues and potential disease triggers. Integrative or functional medicine practitioners are often well-versed in utilizing emerging treatments like low-dose naltrexone and Metformin, which have shown promise in improving immune function and reducing autoimmune antibody levels or bringing in remission of this illness in patients with Hashimoto’s.
Moreover, holistic medicine offers alternative therapies to address stress and mental health concerns associated with Hashimoto’s. It emphasizes personalized nutrition plans, exercise routines, and supplementation strategies tailored to each individual’s needs. The goal is to minimize flare-ups, alleviate symptoms, and enhance overall well-being for those living with Hashimoto’s thyroiditis.
Now, there are a few things I’d like to hear from you:
Have you been diagnosed with Hashimoto’s thyroiditis?
Do you suspect you have this condition but cannot get the proper tests?
If you’ve taken functional/alternative treatments, kindly share which ones worked best for you and weren’t helpful. The information you share will be helpful to others.
References
- Ragusa F, Fallahi P, Elia G, et al. Hashimotos’ thyroiditis: Epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab. 2019;33(6):101367. doi:10.1016/j.beem.2019.101367
- Mincer DL, Jialal I. Hashimoto Thyroiditis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 28, 2021.
- Zaletel K, Gaberšček S. Hashimoto’s Thyroiditis: From Genes to the Disease. Curr Genomics. 2011;12(8):576-588. doi:10.2174/138920211798120763
- Engler H, Riesen WF, Keller B. Anti-thyroid peroxidase (anti-TPO) antibodies in thyroid diseases, non-thyroidal illness and controls. Clinical validity of a new commercial method for detection of anti-TPO (thyroid microsomal) autoantibodies. Clin Chim Acta. 1994;225(2):123-136. doi:10.1016/0009-8981(94)90040-x
- Stephanie L Lee, M.D., 2022. Hashimoto Thyroiditis Treatment & Management: Approach considerations, pregnancy, Myxedema Coma. Hashimoto Thyroiditis Treatment & Management: Approach Considerations, Pregnancy, Myxedema Coma. Available at: https://emedicine.medscape.com/article/120937-treatment [Accessed September 8, 2022].
- Caturegli P, De Remigis A, Rose NR. Hashimoto thyroiditis: clinical and diagnostic criteria. Autoimmun Rev. 2014;13(4-5):391-397. doi:10.1016/j.autrev.2014.01.007
- Caleo A, Vigliar E, Vitale M, et al. Cytological diagnosis of thyroid nodules in Hashimoto thyroiditis in elderly patients. BMC Surg. 2013;13 Suppl 2(Suppl 2):S41. doi:10.1186/1471-2482-13-S2-S41
- Murdaca G, Tonacci A, Negrini S, et al. Emerging role of vitamin D in autoimmune diseases: An update on evidence and therapeutic implications. Autoimmun Rev. 2019;18(9):102350. doi:10.1016/j.autrev.2019.102350
- Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014;18(3):307-309. doi:10.4103/2230-8210.131155
- Gabrielson AT, Sartor RA, Hellstrom WJG. The Impact of Thyroid Disease on Sexual Dysfunction in Men and Women. Sex Med Rev. 2019;7(1):57-70. doi:10.1016/j.sxmr.2018.05.002
- La Vignera S, Vita R. Thyroid dysfunction and semen quality. Int J Immunopathol Pharmacol. 2018;32:2058738418775241. doi:10.1177/2058738418775241
- Harvard Medical School. Thyroid hormone: How it affects your heart
- Li J, Li F. Hashimoto’s Encephalopathy and Seizure Disorders. Front Neurol. 2019;10:440. Published 2019 May 8. doi:10.3389/fneur.2019.00440
- Caleo A, Vigliar E, Vitale M, et al. Cytological diagnosis of thyroid nodules in Hashimoto thyroiditis in elderly patients. BMC Surg. 2013;13 Suppl 2(Suppl 2):S41. doi:10.1186/1471-2482-13-S2-S41
- Ch’ng CL, Jones MK, Kingham JG. Celiac disease and autoimmune thyroid disease. Clin Med Res. 2007;5(3):184-192. doi:10.3121/cmr.2007.738
- Ginanjar E, Sumariyono, Setiati S, Setiyohadi B. Vitamin D and autoimmune disease. Acta Med Indones. 2007;39(3):133-141.
- van Zuuren EJ, Albusta AY, Fedorowicz Z, Carter B, Pijl H. Selenium Supplementation for Hashimoto’s Thyroiditis: Summary of a Cochrane Systematic Review. Eur Thyroid J. 2014;3(1):25-31. doi:10.1159/000356040
- Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
- Li Z, You Y, Griffin N, Feng J, Shan F. Low-dose naltrexone (LDN): A promising treatment in immune-related diseases and cancer therapy. Int Immunopharmacol. 2018;61:178-184. doi:10.1016/j.intimp.2018.05.020
- Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014;33(4):451-459. doi:10.1007/s10067-014-2517-2
- Tendon N, Zhang L, Weetman AP. HLA Associations with Hashimoto’s thyroiditis. Clinical Endocrinology, 1991. 34: 383-386. doi:10.1111/j.1365-2265.1991.tb00309.x
- Bothra N, Shah N, Goroshi M, et al. Hashimoto’s thyroiditis: relative recurrence risk ratio and implications for screening of first-degree relatives. Clin Endocrinol (Oxf). 2017 Aug;87 (2):201-206. doi:10.1111/cen.13323
- Eleftheriou P, Kynigopoulos S, Giovou A. Prevalence of Anti-Neu5Gc Antibodies in Patients with Hypothyroidism. Biomed Res Int. 2014; 2014: 963230. doi:10.1155/2014/963230
- Caturegli P, De Remigis A, Rose NR. Hashimoto thyroiditis: clinical and diagnostic criteria. Autoimmun Rev. 2014 Apr-May;13(4-5):391-7. doi:10.1016/j.autrev.2014.01.007
- Köhling HL, Plummer SF, Marchesi JR, et al. The microbiota and autoimmunity: Their role in thyroid autoimmune diseases. Clin Immunol. 2017 Oct;183:63-74. doi:10.1016/j.clim.2017.07.001
- Brent GA. Environmental Exposures and Autoimmune Thyroid Disease. Thyroid. 2010 Jul; 20(7): 755–761. doi:10.1089/thy.2010.1636
- Jia X, Zhai T, Qu C, et al. Metformin Reverses Hashimoto’s Thyroiditis by Regulating Key Immune Events. Front Cell Dev Biol. 2021;9:685522. Published 2021 May 28. doi:10.3389/fcell.2021.685522. Metformin reduces autoimmune antibody levels in patients with Hashimoto’s thyroiditis.https://www.frontiersin.org/articles/10.3389/fcell.2021.685522/full
Your article provides valuable information about Hashimoto’s symptoms, diagnosis, and management, empowering readers to understand and navigate their health journey effectively. It’s essential to raise awareness about autoimmune thyroid conditions like Hashimoto’s to foster early detection and proper treatment. Thank you for sharing this informative post—it’s sure to make a positive difference in the lives of those affected by Hashimoto Thyroiditis.