
Hashimoto’s thyroiditis is an autoimmune disorder that targets the thyroid gland. In this condition, the immune system mistakenly identifies the thyroid as a threat and begins attacking it, causing gradual destruction of the gland.
As thyroid tissue is progressively damaged, the gland may become unable to produce enough thyroid hormone. The immune system produces antibodies that erroneously target thyroid cells, treating them as foreign invaders like bacteria or viruses. This immune response damages the thyroid cells, leading to hypothyroidism.
Most cases of Hashimoto’s thyroiditis are diagnosed after significant damage has already occurred to the thyroid gland. In this article, I’d like to explore Hashimoto’s thyroiditis in detail and discuss how it can cause an underactive thyroid.
An Overview of Hashimoto thyroiditis
Hashimoto’s thyroiditis is an autoimmune condition that targets and attacks the thyroid gland. It is characterized by the presence of antibodies in the bloodstream that bind to specific components of the thyroid, leading to inflammation.
Over time, the immune system mistakenly identifies parts of the thyroid as foreign invaders and begins attacking the thyroid tissue, treating it as if it were a harmful virus or bacteria. Unfortunately, many conventional doctors and healthcare providers focus primarily on thyroid hormone levels, such as TSH, T3, and T4, often overlooking thyroid antibody testing. This limited approach can make it more difficult to fully assess and treat Hashimoto’s thyroiditis, delaying intervention and allowing irreversible damage to occur in the thyroid gland.
To more accurately diagnose Hashimoto’s thyroiditis, it is crucial for healthcare providers to test not only for thyroid hormones like FT4, FT3, RT3, TSH, and T4, but also for antibodies such as Thyroid Peroxidase Antibodies (TPOAb), Thyroglobulin Antibodies (TgAb), and Thyroid Stimulating Immunoglobulin (TSI). Testing for these antibodies helps rule out both Hashimoto’s thyroiditis and Graves’ disease.
Proper diagnosis of Hashimoto’s thyroiditis requires a comprehensive understanding of its underlying causes and how the condition manifests. Recognizing these factors allows healthcare providers to effectively manage the disease’s symptoms and offer the most appropriate treatments.
Symptoms of Hashimoto’s disease
Hashimoto’s thyroiditis typically develops gradually, progressing over several years. In the early stages, individuals may not experience noticeable signs of the illness. Symptoms can vary significantly from person to person. Because these symptoms overlap with those of other conditions, it is important to consult a certified functional healthcare provider for an accurate diagnosis and effective treatment.
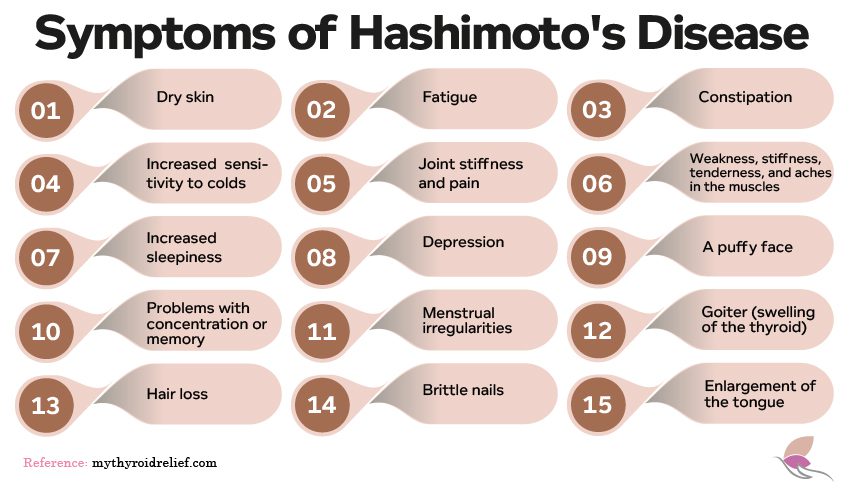
The symptoms associated with Hashimoto’s disease include:
- Dry skin
- Sluggishness fatigue
- Constipation
- Increased sensitivity to cold
- Muscle weakness
- Joint stiffness and pain
- Stiffness, tenderness, and aches in the muscle
- Increased sleepiness
- Depression
- A puffy face
- Problems with concentration or memory
- Excessive or irregular menstrual bleeding
- Goiter (swelling of the thyroid)
- Hair loss
- Brittle nails
- Enlargement of the tongue
Goiters
Hashimoto’s thyroiditis can lead to the development of goiters, which are enlarged thyroid glands. These goiters can result in visible swelling in the neck and may lead to symptoms such as difficulty swallowing or breathing.
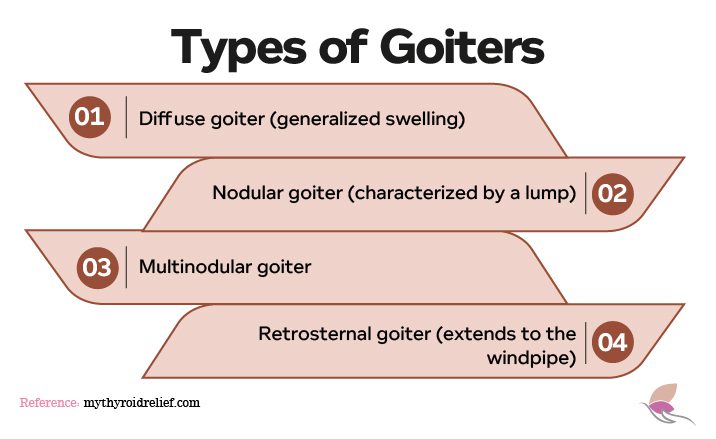
There are four main types of goiters:
- Diffuse goiter: Features smooth, generalized swelling, with uniform enlargement of the entire thyroid gland.
- Nodular goiter: Involves one or more nodules within the thyroid tissue.
- Multinodular goiter: Involves multiple nodules scattered throughout the thyroid gland.
- Retrosternal goiter: Located behind the sternum or breastbone.
How Hashimoto’s Thyroiditis Affects Organs and Systems in the Body
Hashimoto’s thyroiditis is an autoimmune disease that impacts more than just the thyroid. It can affect various organs and systems in the body, leading to a range of symptoms:
- Cardiovascular System: Hashimoto’s can alter heart rate and rhythm, raising the risk of cardiovascular issues such as heart disease and hypertension.
- Cognitive Function: The disease can lead to fatigue, depression, memory problems, and difficulty concentrating, affecting daily mental function.
- Reproductive Health: Hashimoto’s may disrupt menstrual cycles and fertility in women, potentially leading to complications like miscarriage, preterm birth, or preeclampsia during pregnancy.
- Musculoskeletal System: Muscle weakness, joint pain, and stiffness are common, making it harder to carry out everyday tasks.
- Digestive Health: Individuals with Hashimoto’s often experience digestive issues, including constipation, bloating, and abdominal discomfort.
- Skin Health: Hormonal fluctuations from Hashimoto’s can cause skin dryness, itching, and changes in skin texture.
- Metabolism: Hashimoto’s can slow metabolism, leading to weight gain and difficulty losing weight, even with a balanced diet and regular exercise.
- Hormonal Imbalances: Disruptions in thyroid hormone levels can cause secondary imbalances in other hormones, affecting energy levels, mood, and metabolism.
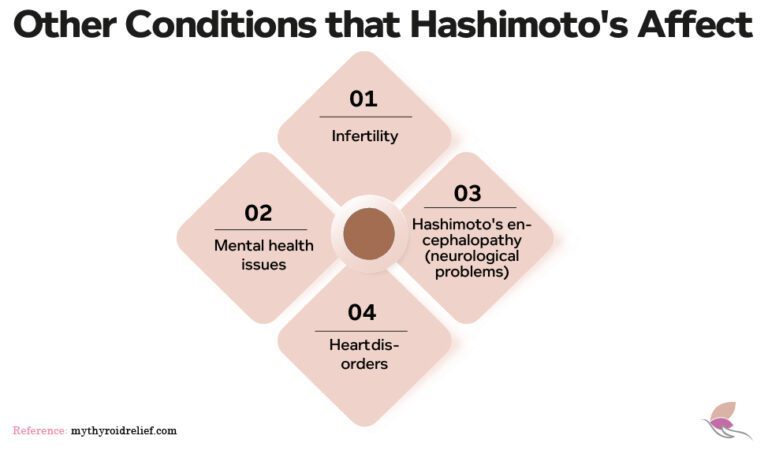
1. Infertility
Women with Hashimoto’s thyroiditis often face fertility challenges, such as difficulties conceiving and an increased risk of miscarriage. Additionally, children born to these women may have a higher risk of congenital disabilities.
Prolactin and testosterone also play a role in autoimmune thyroid diseases. Elevated prolactin levels—often associated with breastfeeding—can occur in women with Hashimoto’s, even if they are not breastfeeding, affecting fertility and thyroid antibody levels. Low testosterone levels, which are linked to an increased risk of autoimmune diseases, may worsen Hashimoto’s symptoms by influencing the body’s inflammatory response.
Thyroid disorders are often linked to sexual dysfunction. Men with hypothyroidism frequently experience erectile dysfunction, reduced libido, delayed ejaculation, and sperm abnormalities. Hyperthyroidism can also reduce semen motility, density, and volume, affecting fertility and sexual health.
2. Heart Disorders
Mild hypothyroidism can significantly affect heart health . For example, it can raise levels of low-density lipoprotein (LDL) cholesterol, commonly known as “bad cholesterol,” due to thyroid hormone imbalance. This increase contributes to arterial hardening, heightening the risk of strokes and heart attacks.
In severe cases, hypothyroidism may lead to pericardial tamponade, a life-threatening condition where the heart struggles to pump enough blood, causing a sharp drop in blood pressure.
A rare but serious complication of hypothyroidism is Hashimoto’s encephalopathy. This condition involves brain inflammation and debilitating neurological symptoms, such as cognitive impairment, seizures, and confusion. It affects approximately two out of every 100,000 people annually, primarily between the ages of 41 and 44 . Females are four times more likely to be affected than males.
3. Hashimoto’s Encephalopathy
Hashimoto’s encephalopathy is a rare and serious neurological complication of Hashimoto’s thyroiditis. This condition arises from inflammation in the brain caused by an autoimmune response, leading to symptoms such as cognitive decline, seizures, and psychiatric disturbances.
Effective treatment often involves corticosteroids to reduce inflammation and suppress the immune system. In cases where symptoms persist, additional therapies, such as immunosuppressive agents, may be required. Early recognition and prompt treatment are essential to prevent lasting neurological damage.
This rare complication highlights the systemic effects of autoimmune thyroid diseases. It underscores the importance of comprehensive evaluation and management to address not only thyroid dysfunction but also its potential impact on the brain and nervous system.
Risk Factors and Triggers for Developing Hashimoto’s Thyroiditis
Researchers and medical professionals have long believed that autoimmune diseases are incurable, with levothyroxine being the primary treatment option. However, early intervention through effective inflammation management, dietary modifications, and individualized treatment strategies can significantly delay or even reverse disease progression.
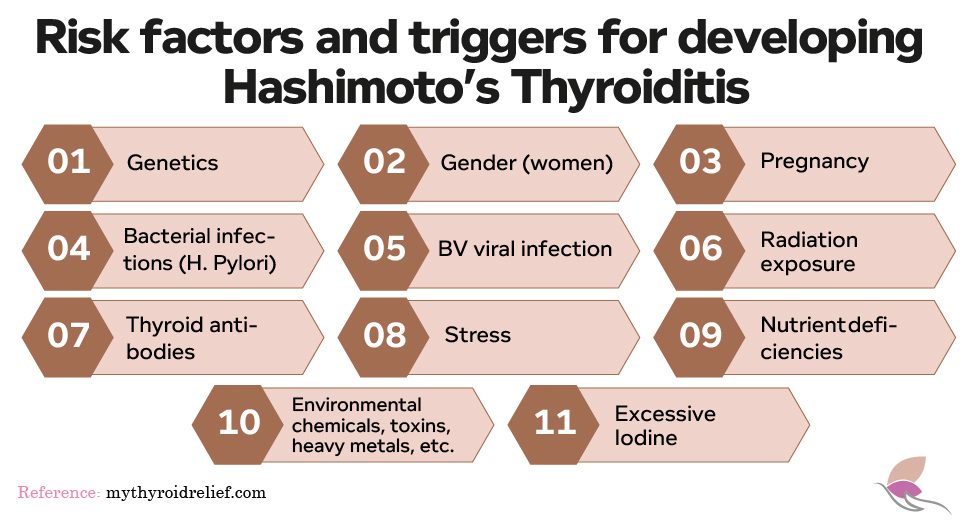
Risk Factors
1. Genetics
Several inherited genes are associated with Hashimoto’s disease. The most commonly linked genes are HLA-DR3 and HLA-DR5, which are typically found in individuals of Caucasian descent. However, having one of these genes does not guarantee the development of Hashimoto’s disease. It merely increases the risk.
Relatives of individuals with Hashimoto’s disease are also at a higher risk. Since Hashimoto’s is more common in women, female relatives have the highest risk. First-degree relatives, especially children, have an incidence rate up to nine times higher than the general population. Furthermore, twins tend to show a higher incidence of Hashimoto’s compared to non-twins.
2. Gender
Women are more likely to develop Hashimoto’s disease than men. Researchers believe that sex hormones like estrogen and progesterone might play a role in making women more prone to this condition. Additionally, some women may experience thyroid issues in the year following childbirth, but these usually resolve on their own. However, in some cases, these postpartum thyroid issues can lead to a diagnosis of Hashimoto’s later in life.
3. Bacterial Infections
Autoimmune diseases, including Hashimoto’s, may be triggered by various infections, such as fungal, parasitic, and yeast infections in the gastrointestinal system. Some individuals may carry these bacteria without showing symptoms. However, more research is needed to understand how specific infections contribute to autoimmune thyroid diseases or how to reduce this risk.
While research suggests a link between autoimmune diseases like Hashimoto’s and gastrointestinal infections, detailed studies on the exact mechanisms and preventive measures are still lacking.
4. Radiation Exposure
Exposure to radiation has been correlated with the development of Hashimoto’s disease. This is particularly evident in cancer patients who undergo radiation treatment and those exposed to nuclear fallout.
5. Thyroid Antibodies
Antibodies associated with Hashimoto’s disease are often present long before a formal diagnosis is made. While test results may initially show normal antibody levels, they may indicate that the thyroid is no longer producing sufficient hormones. Interestingly, around 5% of people with Hashimoto’s disease do not exhibit these antibodies, and those who do tend to have a milder form of the condition.
Potential Triggers of Hashimoto’s
1. Stress
Stress is widely recognized as a factor that can exacerbate symptoms and potentially trigger the onset or worsening of Hashimoto’s thyroiditis. However, it’s important to note that Hashimoto’s is a complex autoimmune condition with multiple contributing factors, and stress is just one part of the picture.
While chronic stress and significant life events can trigger or aggravate autoimmune conditions like Hashimoto’s, other factors—such as genetic predisposition, hormonal imbalances, and environmental influences—also play a role. While eliminating stress completely may not be feasible, adopting healthy stress-management strategies such as meditation, regular exercise, adequate sleep, and seeking emotional support can help mitigate its impact on health.
2. Epstein-Barr Virus (EBV)
The Epstein-Barr virus (EBV), a member of the herpes virus family, is linked to the development of Hashimoto’s thyroiditis. Once infected, EBV remains dormant in the body, but it can reactivate under certain conditions, such as stress, weakened immunity, or hormonal fluctuations. When reactivated, EBV can trigger or worsen Hashimoto’s symptoms by impacting the immune system.
3. Helicobacter Pylori
Helicobacter pylori is a type of bacteria commonly found in the stomach and known for its role in causing stomach ulcers. However, it also affects the immune system and has been associated with Hashimoto’s thyroiditis. Over 50% of the global population is infected with H. pylori, and treatments that reduce stomach acid can increase the risk of infection.
4. Nutrient Deficiencies
Certain nutrient deficiencies can exacerbate Hashimoto’s disease symptoms or flare-ups. Essential nutrients like vitamins D and B12, as well as minerals such as zinc, magnesium, selenium, and iodine, play vital roles in thyroid function and overall immune health.
For instance, vitamin D deficiency has been shown to weaken the immune system, increasing susceptibility to infections and stress. Other beneficial nutrients for thyroid health include:
- Glutathione
- Probiotics
- B-complex vitamins (B1, B12)
- Curcumin
- L-Carnitine
- Magnesium (taken at least 4 hours after thyroid medication)
- Fish oil (from Alaska salmon)
- Iron
In addition to these, supplements like alpha-lipoic acid and N-acetyl cysteine may provide benefits for individuals with Hashimoto’s. It is essential to have regular tests for nutrient deficiencies and to work with a doctor to ensure safe and effective supplementation.
It’s crucial to remember that excessive intake of these nutrients can lead to negative health effects, and taking periodic breaks from supplementation is important to avoid disrupting hormonal balance.
5. Bacterial/Fungal Overgrowth Syndromes (SIBO & SIFO)
Small Intestinal Bacterial Overgrowth (SIBO) and Small Intestinal Fungal Overgrowth (SIFO) are gut conditions that highlight the importance of gut health in autoimmune diseases like Hashimoto’s. The gut is not only vital for nutrient absorption but also plays a central role in regulating the immune system.
SIBO and SIFO occur when there’s an imbalance in the gut microbiota, often due to factors like poor diet and stress. Symptoms of these conditions may include:
- Abdominal pain, especially after eating
- Diarrhea
- Bloating
- Cramps
- Indigestion
- Gas
- A feeling of fullness
These symptoms can worsen in individuals with thyroid conditions since hypothyroidism slows down gut motility, increasing the risk of SIBO. If you suspect SIBO or SIFO, consult a healthcare provider for testing and treatment.
6. Environmental Factors
Environmental factors, including toxins and heavy metals, can damage the thyroid and contribute to autoimmune diseases like Hashimoto’s. These toxins can be found in food, personal care products, household items, dental work, and even in chemicals used in swimming pools and hot tubs.
Other factors, such as vaccines, pregnancy, excessive iodine intake, and radiation exposure, may also trigger autoimmune illnesses like Hashimoto’s.
Diagnosis of Hashimoto Thyroiditis
Diagnosing Hashimoto’s thyroiditis is crucial because it shifts the approach to treatment. For regular hypothyroidism, thyroid hormone replacement is often sufficient. However, Hashimoto’s patients may require lifelong thyroid medication, and early intervention can delay or even prevent this need. Detecting the condition early also helps to slow or reverse the disease’s progression, protecting the thyroid from long-term damage.
Why is this important? Many doctors focus only on thyroid function tests and delay treatment until significant gland impairment occurs. By this point, patients are already experiencing symptoms such as fatigue, hair loss, cold intolerance, and weight gain. Unfortunately, diagnosing Hashimoto’s is often dismissed as unnecessary because it doesn’t alter the standard treatment plan.
This “wait-and-see” approach leaves the thyroid gland vulnerable to continued autoimmune attacks until medication becomes inevitable. If this resonates with your situation, take heart, you are not alone. Advocacy for a comprehensive diagnosis is a vital first step toward protecting your thyroid health and seeking tailored treatment options.
Laboratory Tests to Diagnose Hashimoto’s
Diagnosing Hashimoto’s disease often involves a combination of blood tests, imaging, and, in some cases, more invasive procedures. These tests help identify autoimmune activity, assess thyroid function, and confirm the diagnosis. Some are quick and non-invasive, while others require more advanced techniques to provide a clear diagnosis.
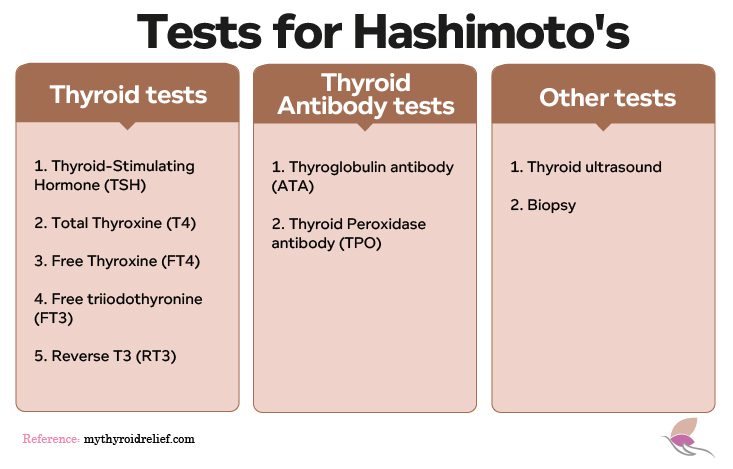
1. Thyroid Function Tests
Thyroid function tests measure hormone levels in your blood to assess how well your thyroid gland is functioning. These tests are crucial for identifying abnormalities in thyroid hormone production and include:
- Total Thyroxine (T4): Measures the total amount of thyroxine hormone, including both bound and unbound forms.
- Free Thyroxine (Free T4): Detects the active, unbound thyroxine hormone, offering a more accurate assessment of thyroid function.
- Free Triiodothyronine (Free T3): Evaluates the level of active thyroid hormone triiodothyronine, which plays a critical role in metabolism.
- Reverse T3: Identifies inactive thyroid hormone levels that may compete with active hormones, providing insight into thyroid metabolism.
- Thyroid-Stimulating Hormone (TSH): Measures TSH production by the pituitary gland. Elevated levels of TSH often indicate hypothyroidism due to Hashimoto’s, as the body tries to stimulate the underactive thyroid.
2. Thyroid Antibody Tests
To confirm Hashimoto’s disease, thyroid antibody tests are used to detect autoimmune activity. These tests are critical for diagnosing the disease, particularly in its early stages:
- Thyroglobulin Antibody (TGAb): Targets thyroglobulin, a protein necessary for thyroid hormone production. Elevated levels suggest autoimmune thyroid damage.
- Thyroid Peroxidase Antibody (TPOAb): Targets thyroid peroxidase, an enzyme essential for hormone synthesis. Increased TPOAb levels are a hallmark of autoimmune thyroid disorders like Hashimoto’s and Graves’ disease.
While these tests are crucial for diagnosing Hashimoto’s, some individuals may show elevated antibody levels without exhibiting symptoms of thyroid dysfunction.
3. Thyroid Ultrasound
A thyroid ultrasound is a non-invasive imaging technique that uses sound waves to create detailed images of the thyroid gland and nearby lymph nodes. This test helps diagnose Hashimoto’s by detecting:
- Increased Blood Flow: Indicative of inflammation from autoimmune activity.
- Gland Enlargement or Shrinkage: Suggestive of thyroid dysfunction.
- Pseudo Nodules: False nodules caused by imaging artifacts that can resemble actual nodules.
A thyroid ultrasound is an effective tool for assessing gland size, structure, and inflammation, providing valuable information without invasive measures.
4. Thyroid Biopsy
A thyroid biopsy is typically reserved for situations where other tests are inconclusive. In this procedure, a small tissue sample is taken from the thyroid gland using a fine needle and examined under a microscope to:
- Confirm Hashimoto’s disease.
- Rule out other thyroid disorders, such as cancer or severe inflammation.
Biopsies are usually performed when additional confirmation is needed before starting treatment.
What is the Link Between Hypothyroidism and Hashimoto’s Disease?
Hashimoto’s disease, also known as chronic lymphocytic thyroiditis, is a prevalent autoimmune condition in which the immune system mistakenly targets and damages the thyroid gland. This immune-mediated destruction gradually impairs the gland’s ability to produce essential hormones, making Hashimoto’s disease the leading cause of hypothyroidism in regions where iodine deficiency is not a concern.
The progression of Hashimoto’s disease is often slow and subtle. Many individuals experience years of thyroid inflammation without noticeable symptoms. Over time, however, the accumulating damage diminishes the thyroid’s ability to function effectively, leading to the hallmark signs of hypothyroidism. This gradual onset frequently complicates early detection and intervention, as symptoms may only emerge once significant damage has occurred.
At the core of Hashimoto’s-induced hypothyroidism is the immune attack on the thyroid gland. This process reduces its capacity to produce thyroxine (T4) and triiodothyronine (T3), hormones critical for regulating metabolism, energy production, and overall bodily functions. When hormone levels drop, the pituitary gland compensates by producing more thyroid-stimulating hormone (TSH). Elevated TSH levels are often the first clinical indicator of hypothyroidism linked to Hashimoto’s disease.
Treatment for Hashimoto’s Thyroiditis
Effective management of Hashimoto’s requires a personalized, holistic approach to alleviate symptoms, prevent complications, and address the underlying autoimmune response. Below is an expanded overview of the treatment options available for managing Hashimoto’s thyroiditis.
1. Conventional Treatment for Hashimoto’s Thyroiditis
Conventional medicine primarily focuses on managing hypothyroidism caused by Hashimoto’s thyroiditis by correcting hormonal imbalances. While medications and regular monitoring are central to this approach, they often do not directly target the autoimmune process responsible for the condition.
Thyroid Hormone Replacement Therapy
The cornerstone of conventional treatment is thyroid hormone replacement therapy, which involves supplementing the hormones that the thyroid no longer produces in adequate amounts.
- Levothyroxine (Synthroid): This synthetic form of thyroxine (T4) is the most commonly prescribed medication. It restores normal thyroid hormone levels in the bloodstream.
- Liothyronine (Cytomel) or Combination Therapy: Some patients may benefit from adding T3 (triiodothyronine) to their treatment plan, particularly if they continue experiencing symptoms despite normal TSH levels. Combination therapy (T4 and T3) is used in such cases.
Monitoring and Dosage Adjustment
Regular monitoring of thyroid function through blood tests is essential to ensure optimal outcomes:
- TSH Levels: Thyroid-stimulating hormone (TSH) levels are closely monitored to maintain proper hormone balance.
- Free T4 and T3 Levels: These tests provide additional insight into thyroid hormone levels.
- Antibodies: Measuring thyroid peroxidase (TPO) antibodies helps assess autoimmune activity.
Frequent blood tests are typically conducted every 6–12 weeks during the initial stages of treatment or when adjusting medication dosages, followed by less frequent monitoring once hormone levels stabilize.
Symptom Management
While thyroid hormone replacement can normalize TSH levels, some patients may still experience symptoms such as fatigue, weight gain, or brain fog. This highlights a limitation of conventional treatment, as it does not address the underlying autoimmune process or other contributing factors like diet and lifestyle.
2. Alternative and Holistic Approaches
Holistic and functional medicine approaches aim to treat Hashimoto’s thyroiditis by addressing the root causes of the autoimmune response. These methods often complement conventional treatments and provide a more comprehensive care plan.
A. Addressing Root Causes
Holistic treatments focus on managing factors that contribute to autoimmune activity and inflammation:
- Chronic Stress: Stress can exacerbate autoimmune conditions by disrupting immune function. Incorporating stress management techniques like meditation, yoga, and therapy can help improve overall well-being.
- Nutrient Deficiencies: Deficiencies in key nutrients such as selenium, zinc, vitamin D, iodine, and magnesium are common in Hashimoto’s patients. Functional practitioners often recommend dietary adjustments or supplements to address these gaps.
- Gut Health: Poor gut health, such as leaky gut syndrome or dysbiosis, is frequently linked to autoimmune diseases. Probiotics, fermented foods, and anti-inflammatory diets can support gut health and help reduce immune system overactivation.
- Environmental Toxins: Reducing exposure to heavy metals, chemicals, and pollutants can minimize triggers for autoimmune responses and improve overall health.
B. Dietary Changes
Diet plays a significant role in reducing inflammation and modulating immune activity. Several dietary approaches are recommended:
- Gluten-Free Diet: Eliminating gluten has been shown to reduce inflammation, particularly in individuals with gluten sensitivity and autoimmune conditions.
- Autoimmune Protocol (AIP): This strict elimination diet removes common food triggers like gluten, dairy, soy, and processed foods while focusing on nutrient-dense, whole foods.
- Mediterranean Diet: Known for its anti-inflammatory properties, the Mediterranean diet emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats like olive oil and omega-3 fatty acids.
- Dairy-Free Diet: Avoiding dairy may help alleviate inflammation and improve symptoms in some individuals with Hashimoto’s.
C. Stress and Lifestyle Management
Chronic stress can worsen autoimmune conditions. A balanced lifestyle, including mindfulness, adequate sleep, regular exercise, and relaxation techniques, is essential for managing Hashimoto’s.
D. Supplements and Natural Support
Certain supplements may support thyroid function and immune health:
- Selenium: Helps reduce TPO antibodies and supports thyroid function.
- Vitamin D: Regulates immune function and may reduce autoimmunity.
- Omega-3 Fatty Acids: Anti-inflammatory properties of omega-3s found in fish oil help manage symptoms.
- Probiotics: Improve gut health, support immune resilience, and reduce inflammation.
3. Remission
In some cases, Hashimoto’s thyroiditis can be managed to the point of remission, particularly with a functional medicine approach. Remission is characterized by a reduction in symptoms, a decrease in thyroid antibody levels, and minimized autoimmune activity. The process typically involves:
- Identifying and Eliminating Triggers: This includes avoiding food intolerances, infections, or environmental toxins.
- Adopting a Personalized Plan: Tailoring diet, lifestyle, and stress management strategies to individual needs can help.
- Working with Healthcare Providers: Addressing stress, gut health, and nutrient deficiencies with a functional medicine practitioner can support the healing process.
4. Integrating Conventional and Holistic Treatments
Many patients benefit from combining conventional and holistic treatments for Hashimoto’s thyroiditis. This integrated approach addresses both the symptoms and the underlying causes of the condition:
- Conventional Medicine: Stabilizes TSH levels through thyroid hormone replacement therapy.
- Holistic Methods: Reduce inflammation, improve gut health, and address root causes of autoimmune activity.
Collaborating with an integrative or functional medicine practitioner can help create a personalized treatment plan that incorporates both conventional and holistic strategies for optimal results.
5. Importance of Early Diagnosis and Ongoing Monitoring
Early diagnosis of Hashimoto’s thyroiditis is crucial to prevent complications such as goiter, infertility, or cardiovascular issues. Regular monitoring of thyroid function and autoimmune activity is vital for tracking disease progression and ensuring effective management. By integrating conventional treatments with holistic strategies, patients can achieve better symptom management, improve quality of life, and potentially achieve remission.
Vitamins and Minerals for Hashimoto’s Disease
Vitamins and minerals play a crucial role in supporting thyroid health and immune function in individuals with Hashimoto’s disease.
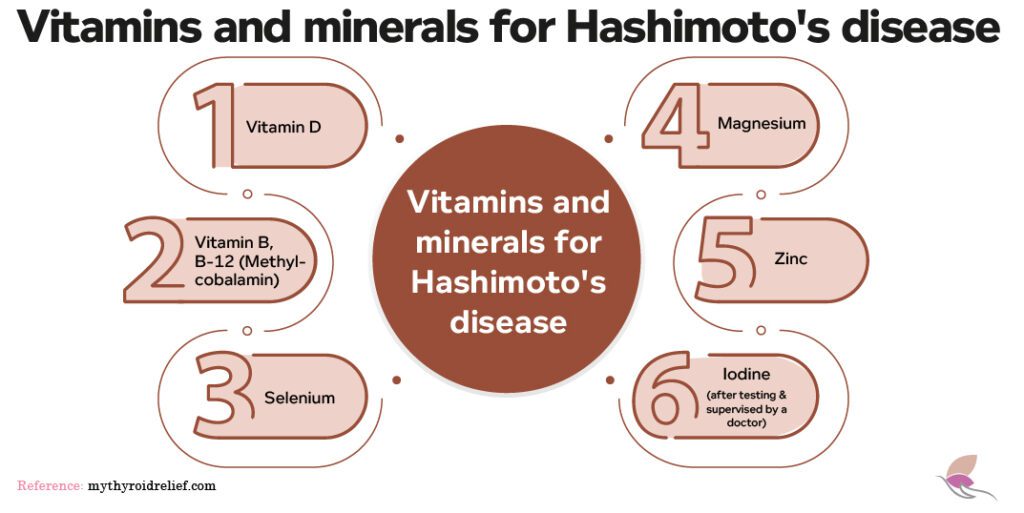
Here are some key nutrients that can help manage the condition:
-
Vitamin D
Vitamin D is essential for regulating the immune system and can help reduce autoimmune activity in Hashimoto’s disease. Low levels of vitamin D are common in people with autoimmune disorders, and supplementation may improve immune function, reduce inflammation, and support thyroid health.
-
Vitamin B Complex (Including B-12)
Vitamin B12 is often deficient in individuals with Hashimoto’s, contributing to fatigue, cognitive issues, and mood disturbances. A B-complex supplement, including B12, can help improve energy levels, support neurological health, and enhance thyroid hormone production.
-
Selenium
Selenium acts as an antioxidant and plays a key role in thyroid hormone metabolism. Studies suggest that selenium supplementation can reduce thyroid peroxidase (TPO) antibodies, which are often elevated in Hashimoto’s patients. Selenium also helps protect the thyroid gland from oxidative stress, which can damage thyroid cells.
-
Magnesium
Magnesium is involved in over 300 biochemical reactions in the body, including regulating thyroid hormone function. Magnesium can help alleviate symptoms commonly associated with Hashimoto’s, such as fatigue, muscle cramps, and irritability. It also supports stress management, which is vital for those dealing with autoimmune thyroid conditions.
-
Zinc
Zinc supports thyroid hormone production by facilitating the conversion of inactive thyroid hormone (T4) into its active form (T3). A zinc deficiency can impair thyroid function and exacerbate symptoms of hypothyroidism. Zinc also supports immune health, which is crucial in managing autoimmune diseases like Hashimoto’s.
-
Iodine
Iodine is necessary for the production of thyroid hormones. However, both iodine deficiency and excess iodine can trigger or worsen autoimmune thyroid disorders like Hashimoto’s. It is essential to monitor iodine intake carefully, as inappropriate supplementation can lead to complications.
Supplements for Hashimoto’s Disease
Supplements are an important part of managing Hashimoto’s disease, particularly when it comes to addressing nutrient deficiencies and supporting overall thyroid health.
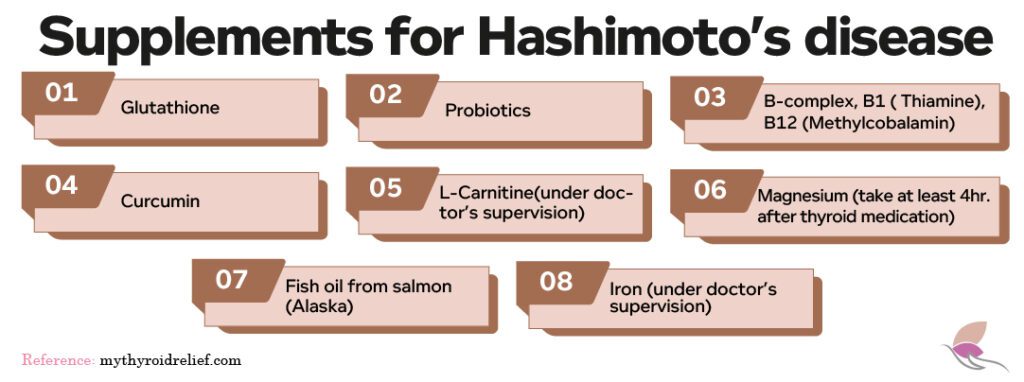
Here are some supplements commonly recommended for individuals with Hashimoto’s:
1. Glutathione
Glutathione is an antioxidant that helps protect the thyroid gland from oxidative damage. Supplementing with glutathione may reduce inflammation, support thyroid health, and improve overall immune function.
2. Probiotic
Since gut health is crucial for immune function, probiotic supplements can help improve the gut microbiome and reduce inflammation. A healthy gut can support immune tolerance and potentially reduce autoimmune flare-ups, which are common in Hashimoto’s disease.
3. Vitamin B12
B vitamins, especially B12, are important for managing fatigue and cognitive issues often seen in Hashimoto’s patients. A B-complex supplement can support energy production, improve mental clarity, and help with thyroid hormone regulation.
4. Curcumin
Curcumin, derived from turmeric, has anti-inflammatory properties that can help reduce the inflammation and oxidative stress often seen in Hashimoto’s patients. Supplementing with curcumin may help manage symptoms and support thyroid health.
5. Zinc and Magnesium
Both zinc and magnesium support thyroid hormone production and help alleviate common symptoms like fatigue, brain fog, and muscle cramps, which are often associated with Hashimoto’s disease. Zinc also supports the conversion of T4 to T3, the active thyroid hormone.
6. Fish Oil (Omega-3 Fatty Acids)
Fish oil supplements provide essential omega-3 fatty acids, which are anti-inflammatory and beneficial for overall immune function. Omega-3s support thyroid function and can help reduce autoimmune responses associated with Hashimoto’s disease.
7. Iron Supplements
Many people with Hashimoto’s disease experience iron deficiency, which can exacerbate fatigue and other symptoms. Supplementing with iron can help restore energy levels and support thyroid function.
8. L- Carnitine
L-carnitine is an amino acid derivative that plays a role in energy production. Studies suggest that L-carnitine can help alleviate symptoms of fatigue and muscle weakness often experienced by individuals with hypothyroidism and Hashimoto’s.
References
- https://my.clevelandclinic.org/health/diseases/17665-hashimotos-disease
- https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/symptoms-causes/syc-20351855
- https://www.webmd.com/women/hashimotos-thyroiditis-symptoms-causes-treatments
- https://www.thyroid.org/hashimotos-thyroiditis/