
Hyperthyroidism and Graves’ disease are medical conditions characterized by the overproduction of thyroid hormones by the thyroid gland. These conditions can result in symptoms ranging from mild discomfort to severe health complications. In this article, we will explore the details of hyperthyroidism and its connection to Graves’ disease, aiming to empower individuals to make informed decisions about their health.
What Is Hyperthyroidism?
Hyperthyroidism is a condition where the thyroid gland produces excess thyroid hormone, disrupting the body’s metabolism, energy levels, and overall health. Since the thyroid regulates many vital bodily functions, any imbalance in its hormone production can have significant effects.
Types of Hyperthyroidism
1. Primary Hyperthyroidism
Primary hyperthyroidism occurs when the thyroid gland itself produces excessive thyroid hormone. This can be caused by thyroid nodules, inflammation, or autoimmune diseases, leading to hormone overproduction without external stimulation.
2. Secondary Hyperthyroidism
Secondary hyperthyroidism occurs when the thyroid is overstimulated by excess thyroid-stimulating hormone (TSH), often due to issues with the pituitary gland. The pituitary releases TSH, prompting the thyroid to produce more hormones than necessary. Managing the underlying pituitary condition is essential for controlling secondary hyperthyroidism.
What Is Thyrotoxicosis?
Thyrotoxicosis refers to elevated thyroid hormone levels in the bloodstream, regardless of the source. It can result from conditions such as thyroid nodules, Graves’ disease, or other underlying issues.
Symptoms of Hyperthyroidism and Thyrotoxicosis
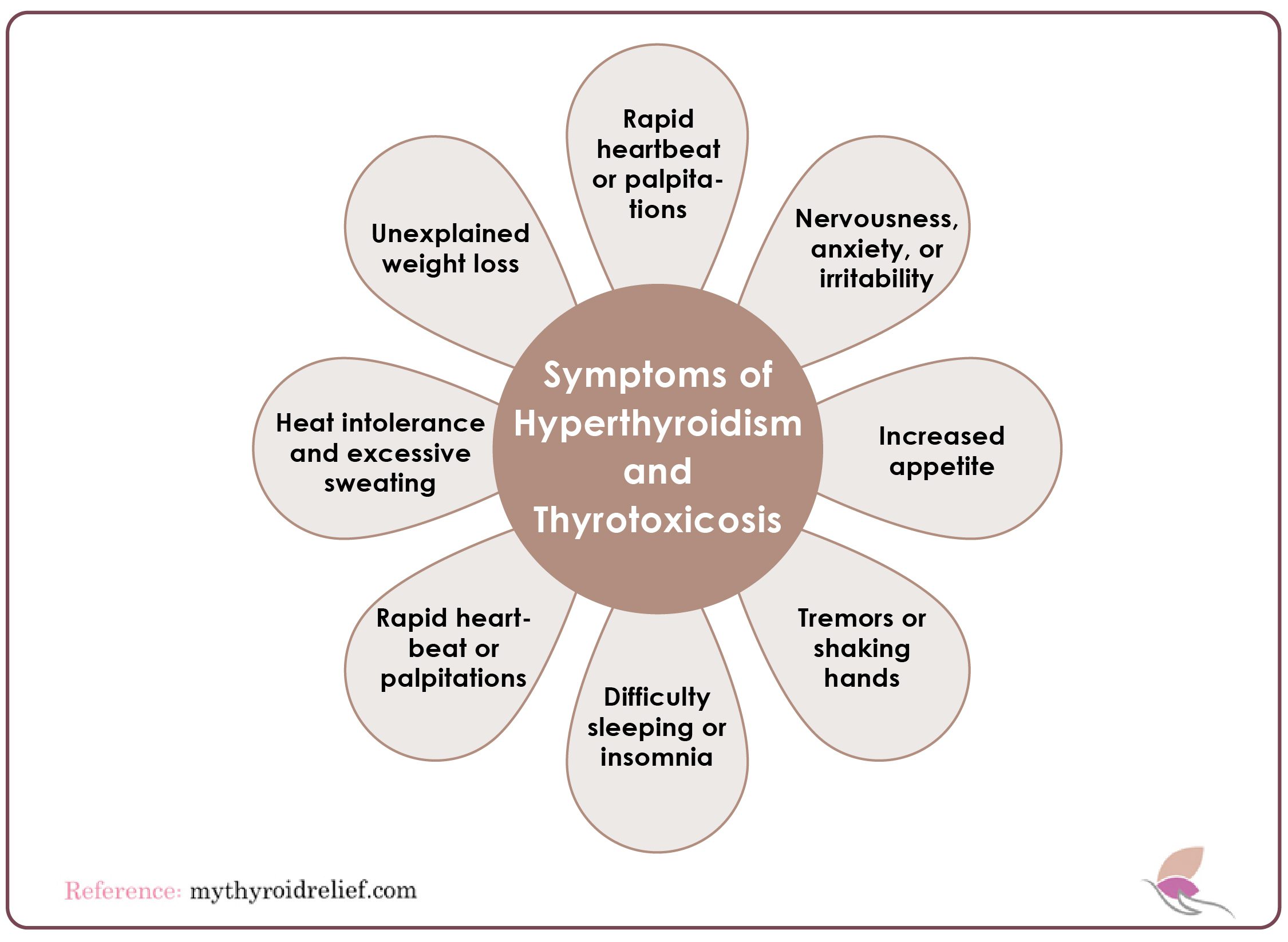
Both hyperthyroidism and thyrotoxicosis share common symptoms, which can range from mild to severe and may worsen over time if untreated. These symptoms include:
- Rapid heartbeat or palpitations
- Unexplained weight loss
- Heat intolerance and excessive sweating
- Nervousness, anxiety, or irritability
- Increased appetite
- Tremors or shaking hands
- Difficulty sleeping or insomnia
Understanding Graves’ Disease
Graves’ disease is an autoimmune condition that affects the thyroid gland, often leading to hyperthyroidism and gland enlargement. If left untreated, this disorder can pose lifelong risks and may even result in severe health complications, including death. However, with adequate treatment, the disease can be effectively managed, and in some cases, it may even go into remission.
In Graves’ disease, the immune system mistakenly attacks the thyroid-stimulating hormone receptors (TSH-R) on the thyroid gland, causing the gland to become overactive.
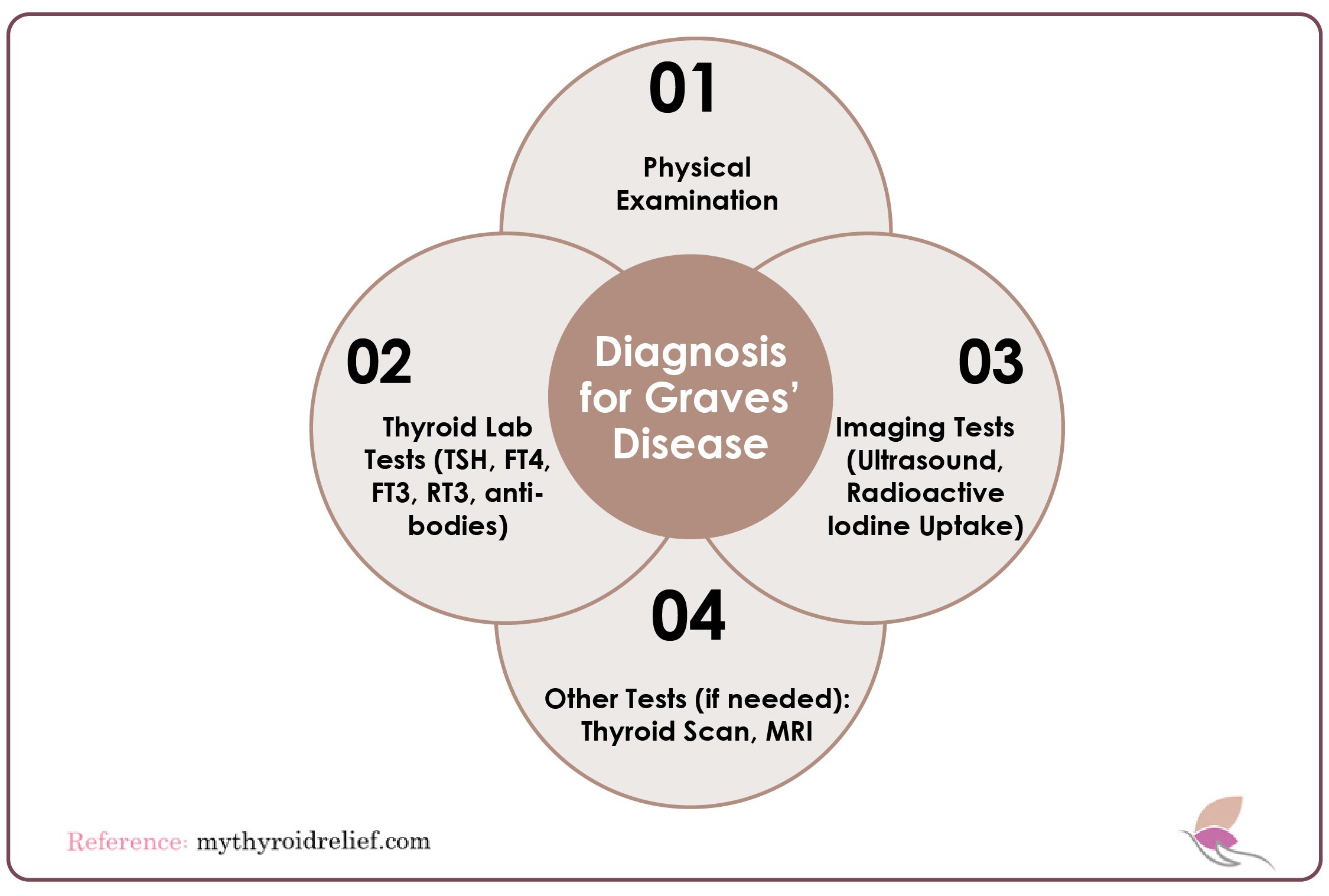
Diagnosis Of Graves’ Disease
Graves’ disease diagnosis is typically straightforward. There are three main ways it can be done:
1. Physical Examination
The physical examination helps identify visible symptoms of Graves’ disease, such as an enlarged thyroid (goiter), bulging eyes (exophthalmos), and skin changes. The doctor will assess the patient’s overall health, check the thyroid gland for enlargement, and evaluate any symptoms related to hyperthyroidism.
2. Thyroid Lab Tests
The laboratory tests most helpful for diagnosing patients with Graves’ disease include the free TSH, free T4 (FT4), free T3 (FT3), and TSI tests.
- Free T4 Test: The Free T4 test measures thyroxine that is available to the body’s cells. FT4 levels are increased in hyperthyroidism and thyroid hormone resistance.
- Free T3 Test: The Free T3 test measures triiodothyronine that is free in the body, and it is elevated in Graves’ disease.
- TSH Test: The thyroid-stimulating hormone (TSH) signals the thyroid gland to produce hormones that regulate metabolism. A TSH test can reveal whether your thyroid gland is functioning at normal levels. In Graves’ disease, TSH levels are typically lower than normal, which disrupts thyroid function.
- Thyroid Peroxidase (TPO) Antibody Test: This blood test measures a specific type of thyroid antibody produced in response to thyroid inflammation. It helps differentiate between Graves’ disease and hyperthyroidism caused by toxic nodular goiter. It may also confirm that goiter and/or hypothyroidism are due to autoimmune thyroiditis. The typical range for TPO antibodies is below 2 IU/mL.
- Thyrotropin (TSH) Receptor Antibody Test: A high result in the Thyrotropin (TSH) receptor antibody test indicates the presence of antibodies targeting the TSH receptor, suggesting Graves’ disease.
3. Imaging Tests (Ultrasound, Radioactive Iodine Uptake)
Imaging tests are used to confirm the diagnosis of Graves’ disease and assess thyroid function. An ultrasound can evaluate the size and texture of the thyroid gland. At the same time, the Radioactive Iodine Uptake (RAIU) test measures how much iodine the thyroid absorbs, which is typically increased in cases of Graves’ disease.
4. Other Tests (if needed): Thyroid Scan, MRI
A thyroid scan involves a small amount of radioactive iodine to evaluate the thyroid’s structure and function. An MRI will assess eye involvement, particularly in cases where Graves’ disease affects the orbits (exophthalmos). This is usually done if there are signs of eye problems or if more detailed imaging is needed.
Causes of Graves’ Disease
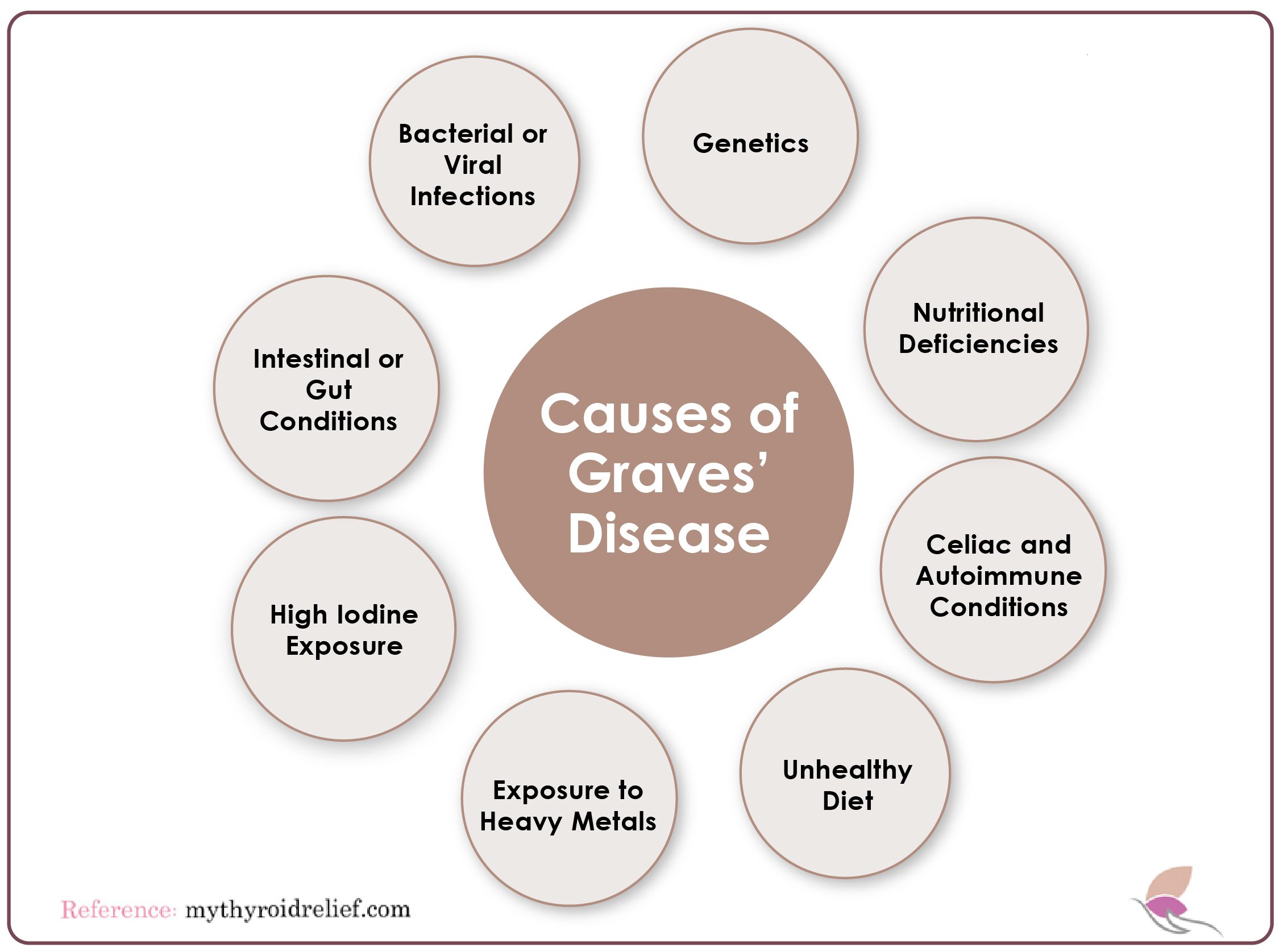
1. Bacterial or Viral Infections
Infections can significantly impact the immune system, causing it to produce antibodies that target the thyroid gland. For instance, H. pylori, a bacterium known for causing gastrointestinal issues, has been linked to autoimmune responses like Graves’ disease. Research suggests that H. pylori infection may trigger molecular mimicry, where the immune system mistakenly attacks thyroid tissue.
Similarly, infections caused by Yersinia enterocolitica (often contracted from consuming raw or undercooked pork) have also been associated with Graves’ disease, further demonstrating the connection between microbial triggers and autoimmune thyroid disorders.
2. Genetics
Genetics play a significant role in the development of Graves’ disease, although they cannot be controlled. Individuals with a genetic predisposition may inherit genes associated with the disease, but environmental factors must also be present to trigger its development—a phenomenon known as multifactorial inheritance. Several genes have been linked to Graves’ disease, including those that affect the immune system, such as CD25, CD40, CTLA-4, FOXP3, and HLA-DR3.
Additionally, genes directly related to thyroid function, such as thyroglobulin (Tg) and the thyroid-stimulating hormone receptor (TSHR), are also implicated in Graves’ disease. Modifier genes may further influence the disease’s development, but the precise mechanisms remain incompletely understood.
3. Intestinal or Gut Conditions
The gut plays a crucial role in immune system interactions. Intestinal hyperpermeability (commonly known as leaky gut), food allergies (especially gluten), and microbial imbalances in the gut can lead to systemic inflammation. This inflammation may activate the immune system, contributing to the onset and progression of Graves’ disease.
4. Nutritional Deficiencies
Nutritional deficiencies, particularly in iodine, selenium, zinc, and vitamin D, can impair thyroid function and immune regulation, increasing the risk of Graves’ disease. Gluten intolerance may also trigger thyroid-related antibodies, worsening the condition.
A poor diet high in refined foods, caffeine, alcohol, trans fats, and added sugars can promote inflammation and aggravate symptoms. Instead, a nutrient-rich diet focusing on whole foods, organic vegetables, grass-fed meats, antioxidant-rich fruits (like berries), and healthy fats (such as avocado, coconut, and olive oil) is recommended.
Avoiding gluten-containing grains like wheat, rye, and barley and identifying food allergies or sensitivities can further reduce inflammation and support thyroid health.
5. High Iodine Exposure
Excessive iodine exposure is known to contribute to Graves’ disease. Additionally, individuals with the condition often experience deficiencies in essential nutrients like vitamins C, D, E, selenium, magnesium, and B-complex vitamins. Of particular importance is Vitamin B12, as many patients with Graves’ disease produce anti-parietal cell antibodies, which block the absorption of B12.
These antibodies, common in autoimmune thyroid disorders, can hinder the body’s ability to absorb vital nutrients, necessitating B12 injections or sublingual supplementation.
6. Exposure to Heavy Metals
Heavy metals like mercury and lead can disrupt immune system function and thyroid health, potentially increasing the risk of autoimmune disorders such as Graves’ disease.
7. Unhealthy Diet
A diet lacking in essential nutrients, such as iodine, selenium, or zinc, can impair thyroid function and immune health, making individuals more vulnerable to developing autoimmune thyroid disorders. Additionally, diets high in processed foods and sugar may contribute to inflammation, which can exacerbate autoimmune conditions.
8. Celiac Disease and Autoimmune Conditions
Studies suggest that individuals with Graves’ disease may be up to 4.5 times more likely to develop celiac disease or other autoimmune conditions compared to those without Graves’ disease. This highlights the importance of monitoring for additional autoimmune disorders in patients diagnosed with Graves’ disease.
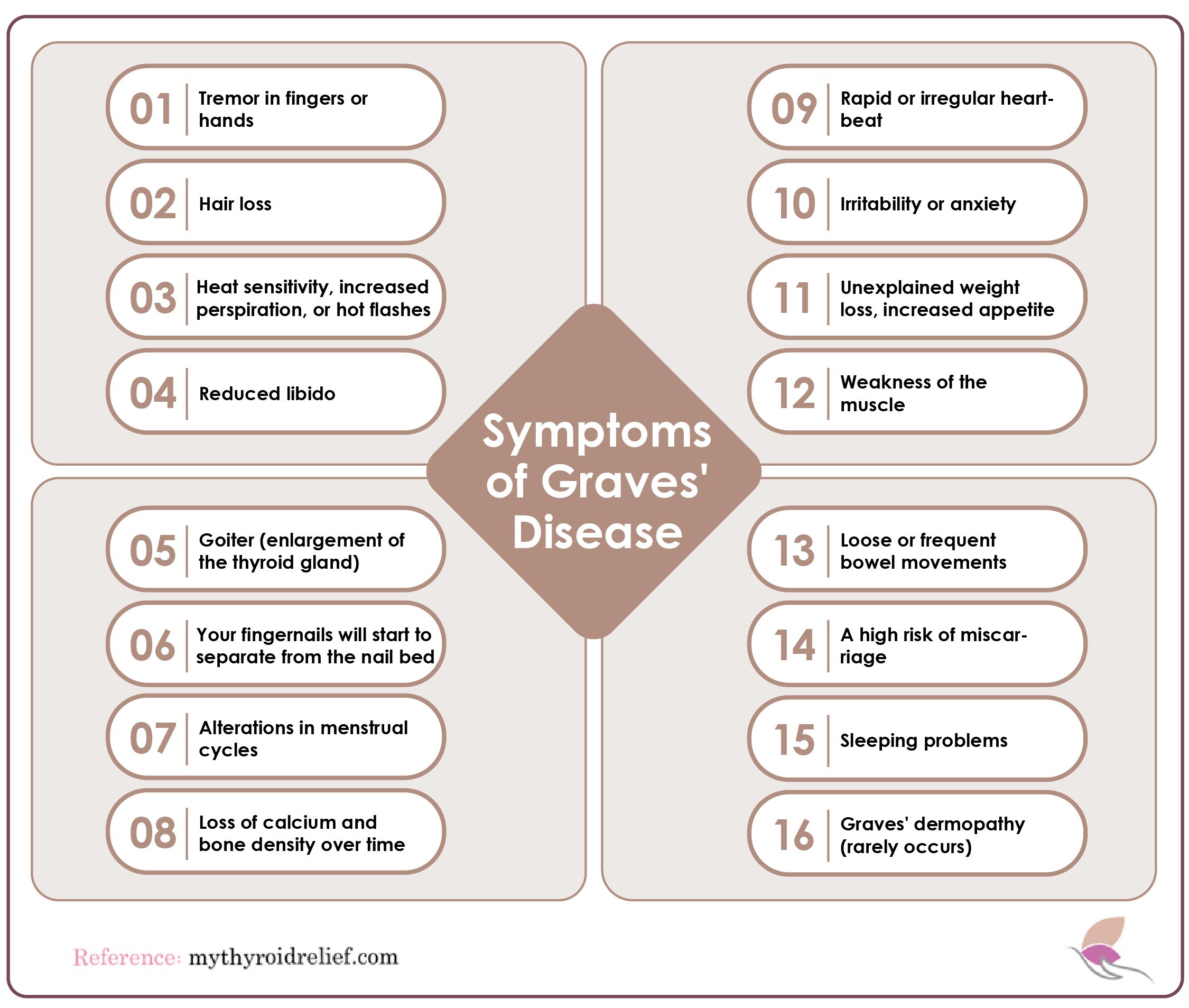
Symptoms of Graves’ Disease
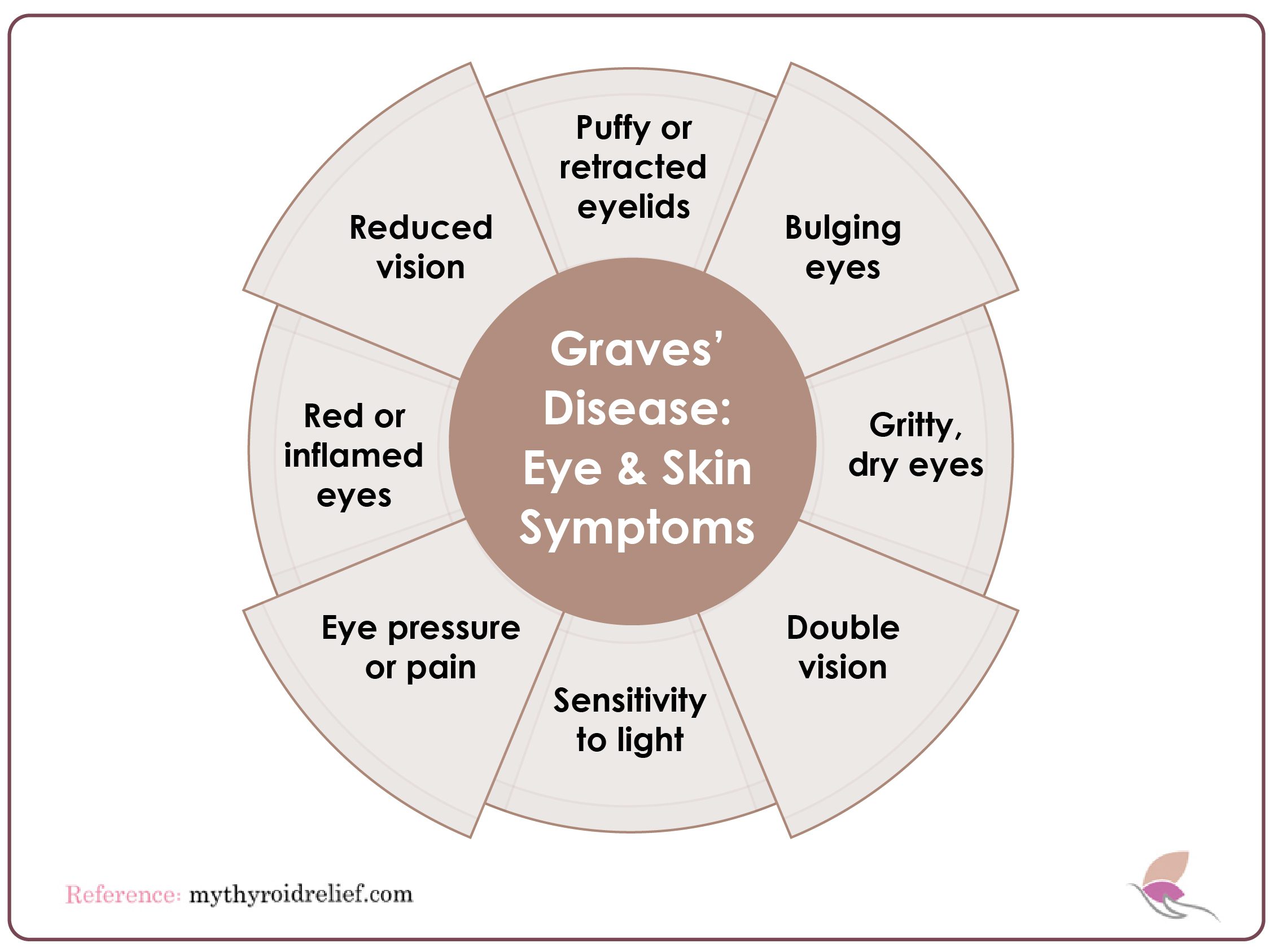
1. Graves’ Ophthalmopathy (Thyroid Eye Disease)
Graves’ ophthalmopathy, also called thyroid eye disease, affects more than half of those with Graves’ disease. It occurs when the immune system attacks the muscles and tissues around the eyes, causing inflammation. Severe cases, affecting 3-5% of patients, can lead to significant eye problems, including:
- Puffy or retracted eyelids: The upper eyelids may appear swollen or pulled back.
- Bulging eyes (exophthalmos): The eyes protrude due to swelling behind them.
- Gritty sensation in the eyes: Dry, irritated eyes are common due to inflammation.
- Double vision: Swelling can affect eye muscles, leading to misalignment and blurred or double vision.
- Sensitivity to light: The eyes may become extremely sensitive to bright light.
- Pressure or pain in the eyes: A feeling of tightness or discomfort in and around the eyes.
- Red or inflamed eyes: The whites of the eyes may appear red or bloodshot.
- Reduced vision: In severe cases, patients may experience diminished vision or even vision loss.
2. Graves’ Dermopathy
Graves’ dermopathy, though less common, is another manifestation of the disease. It usually presents as thickened, red, and swollen patches of skin, often on the shins or feet. While typically painless, it can cause discomfort, itching, or tenderness. Treatment generally involves topical corticosteroids to reduce inflammation, although more aggressive treatments may be necessary for severe cases.
Thyroid Storm: Causes, Symptoms, and Diagnosis
A thyroid storm is a rare but life-threatening complication of hyperthyroidism, often associated with unmanaged Graves’ disease. In this emergency, an overwhelming amount of thyroid hormones triggers dangerous spikes in heart rate, blood pressure, and body temperature. If not treated promptly, this severe response can lead to serious complications. Therefore, managing hyperthyroidism effectively is critical to prevent such emergencies.
Causes of Thyroid Storm
Thyroid storms are rare but potentially life-threatening emergencies that typically occur in patients with hyperthyroidism who have not received adequate treatment. These storms are often triggered by various factors, including:
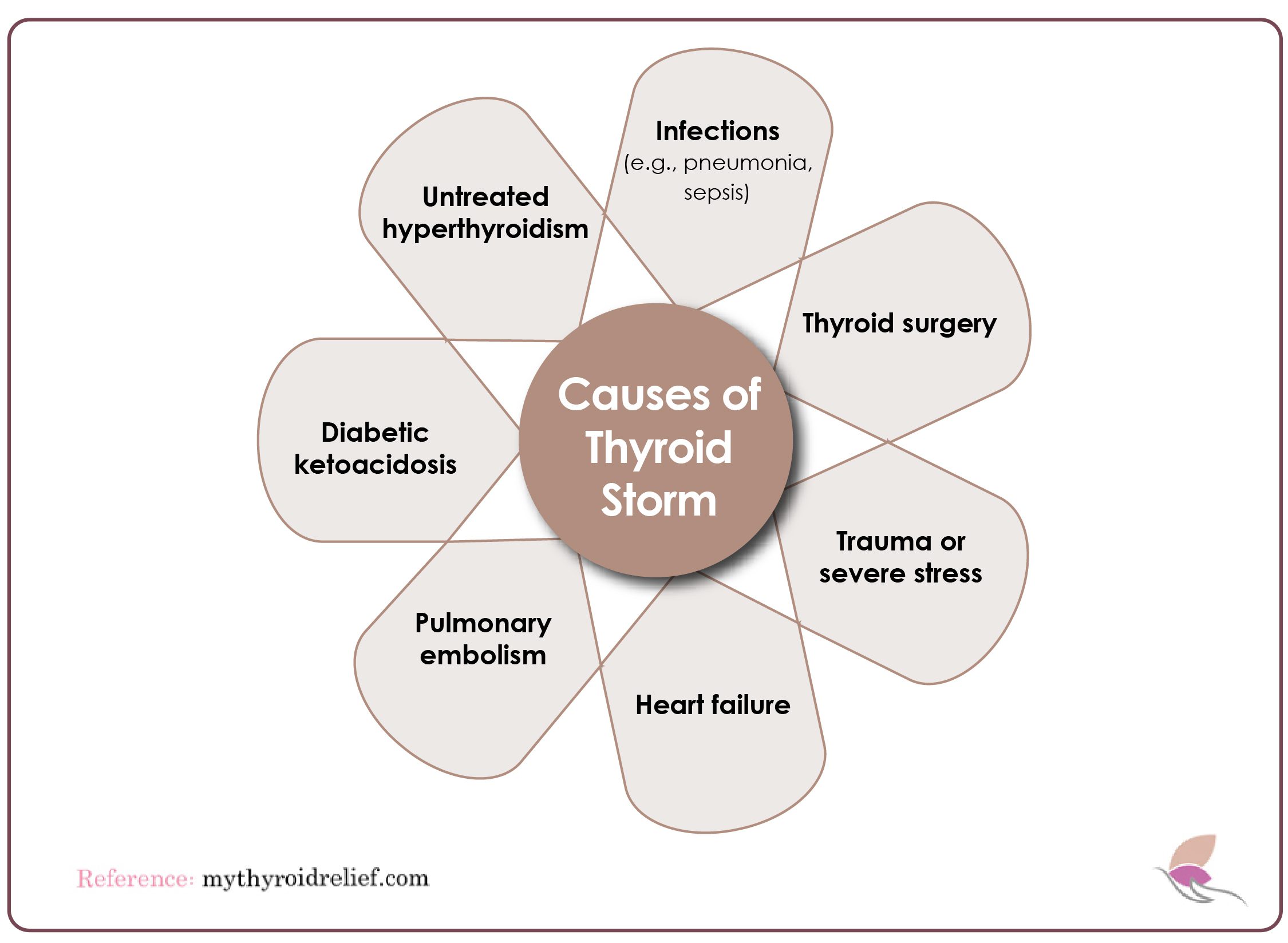
- Untreated or poorly managed hyperthyroidism
- Infections such as pneumonia or sepsis
- Surgical procedures like thyroidectomy (removal of part or all of the thyroid gland)
- Physical trauma or stress
- Heart conditions, such as congestive heart failure
- Pulmonary embolism (a blood clot in the lungs)
- Diabetic ketoacidosis (a complication of diabetes)
Symptoms of Thyroid Storm
Thyroid storms and hyperthyroidism share similar symptoms, but those of a thyroid storm are significantly more severe, sudden, and extreme. These intensified symptoms often leave individuals unable to care for themselves. Common signs of a thyroid storm include:
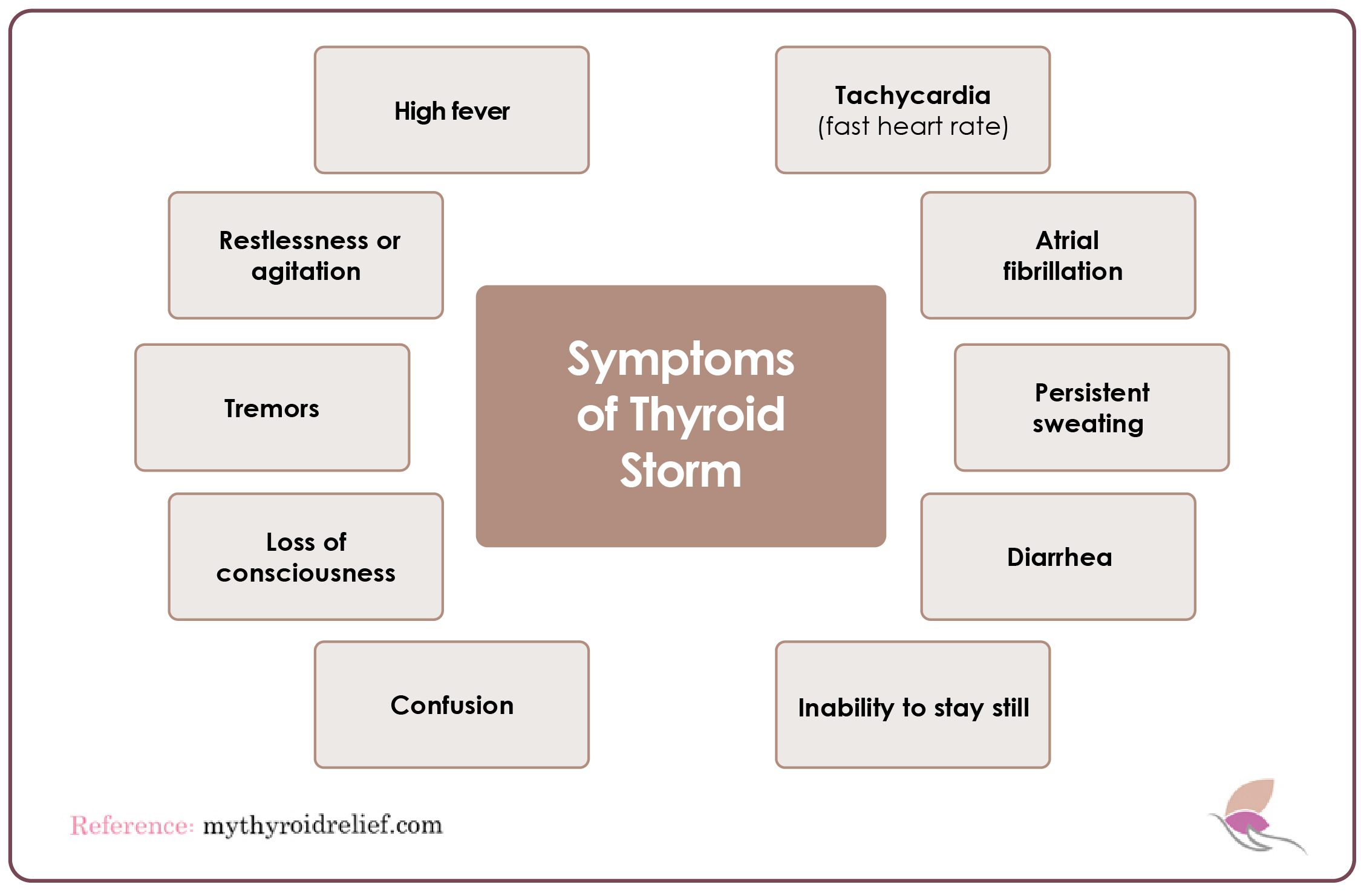
- High fever that escalates rapidly.
- Tachycardia (rapid heart rate) exceeding normal levels.
- Atrial fibrillation is characterized by irregular heart rhythm.
- Restlessness or agitation.
- Tremors or shaking.
- Profuse sweating that persists despite environmental conditions.
- Loss of consciousness or fainting spells.
- Diarrhea is often frequent and urgent.
- Confusion or disorientation.
- Difficulty finding comfort or remaining still.
How is Thyroid Storm Diagnosed?
When individuals with hyperthyroidism show signs of a thyroid storm, they are often admitted to the emergency department. Key symptoms include a rapid heartbeat and significantly elevated blood pressure. Your healthcare provider will perform a thorough assessment, which typically involves a blood test to measure thyroid hormone levels.
Those experiencing thyroid storms usually have elevated levels of T3 and T4, while TSH levels typically fall below the normal range, often nearing zero or becoming undetectable. This contrasts with the typical TSH range of 0.4 to 4.0 milli-international units per liter (mIU/L), as indicated by the American Association for Clinical Chemistry (AACC). Holistic doctors now consider the optimal TSH range to be between 0.5 and 1.5 mU/L.
Treatment for Graves’ Disease and Hyperthyroidism
Effective management of Graves’ disease and hyperthyroidism often requires a combination of therapies based on the severity of the condition and the patient’s health status.
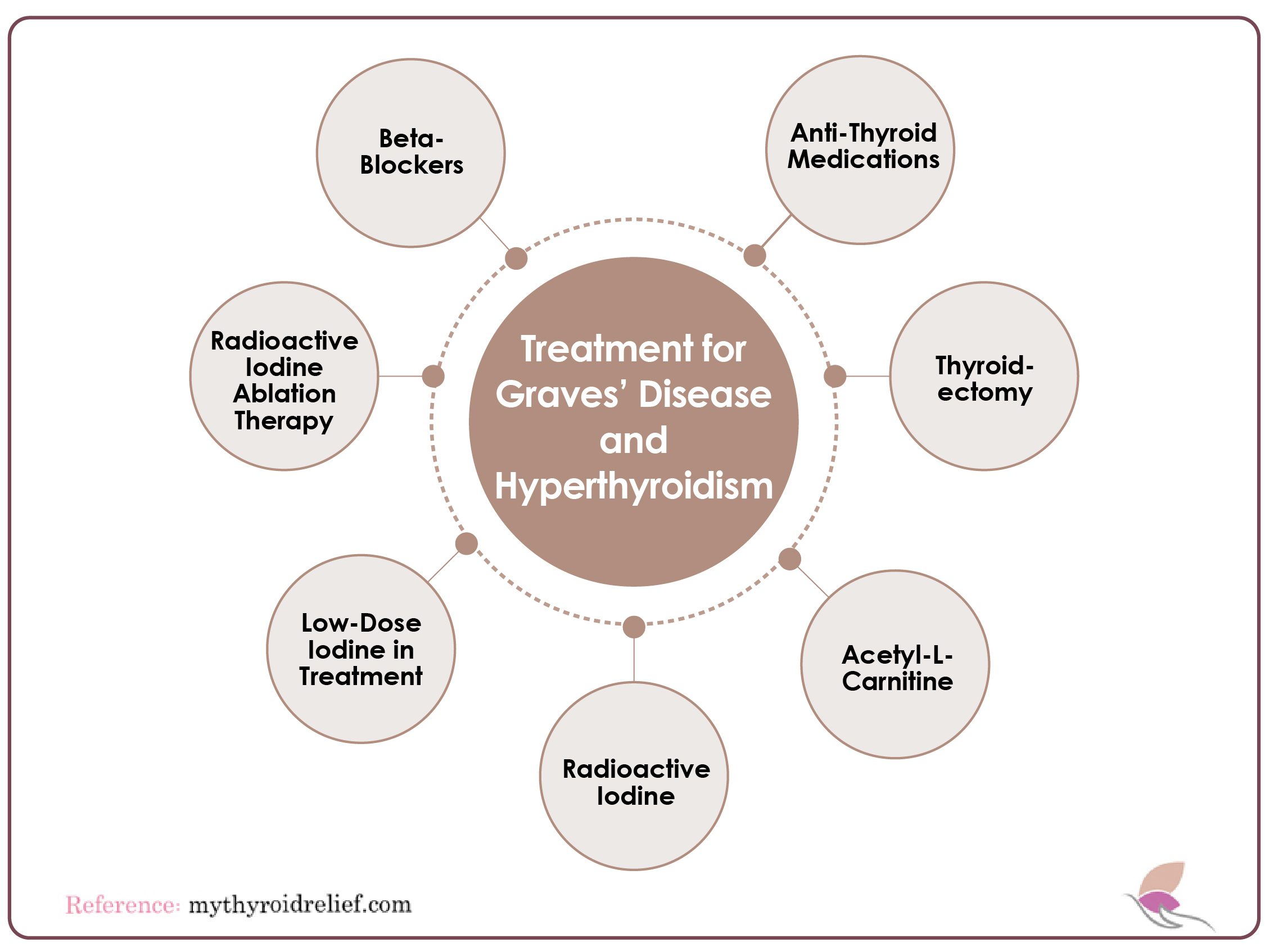
Let’s examine the available treatment options:
1. Beta-Blockers
Beta-blockers, such as propranolol and metoprolol, are frequently the initial treatment for hyperthyroidism and Graves’ disease. While these medications do not reduce thyroid hormone production, they effectively manage symptoms by blocking the effects of excess hormones on the body.
Moreover, by alleviating symptoms like rapid heart rate and anxiety, they can significantly improve quality of life, ultimately contributing to better long-term management. Beta-blockers alleviate Irregular heartbeats, Tremors and muscle weakness, Anxiety or irritability, Heat intolerance and excessive sweating, Diarrhea. Beta-blockers provide rapid symptom relief while more definitive treatments are introduced.
2. Anti-Thyroid Medications
Anti-thyroid drugs like methimazole and propylthiouracil (PTU) are prescribed to inhibit thyroid hormone production. Methimazole is often preferred due to its effectiveness and lower side effect profile, though PTU is used in pregnancy due to its lower risk to the fetus.
Methimazole suppresses thyroid hormone production to below-normal levels, but long-term use may cause liver damage and low white blood cell count. While PTU, though safer during pregnancy, carries a higher risk of liver complications. These medications are generally short-term solutions and may be used to prepare patients for more permanent treatments.
3. Thyroidectomy
For those seeking a long-term cure, thyroidectomy (removal of part or all of the thyroid gland) is a viable option. By eliminating the source of hormone overproduction, the procedure effectively treats hyperthyroidism. However, the surgery carries risks. Hypothyroidism, requires lifelong thyroid hormone replacement therapy. Also, there might be potential damage to nearby structures, such as the parathyroid glands or vocal cords. Despite the risks, thyroidectomy is particularly beneficial for patients unresponsive to medication or with large goiters.
4. Low-Dose Iodine in Treatment
Historically, low-dose iodine has been used to manage hyperthyroidism. Administering controlled doses of iodine helps regulate hormone production, sometimes reducing the need for more invasive treatments. This natural approach is an option for those seeking alternatives to medication; however, supervision by a physician is essential for safety and efficacy. Moreover, professional oversight helps tailor the approach to individual needs.
5. Acetyl-L-Carnitine in Hyperthyroidism Management
Acetyl-L-Carnitine, a dietary supplement, has shown potential in alleviating symptoms associated with hyperthyroidism. It helps regulate thyroid hormone activity, reducing palpitations and rapid heart rate. In studies, L-carnitine has reversed and prevented hyperthyroid symptoms, with patients experiencing reduced palpitations, Improved clinical symptoms, and thyroid function markers.
While promising, it is essential to consult a healthcare provider to determine the appropriate dosage. Additionally, professional guidance ensures safe use, and furthermore, it helps to avoid potential side effects. Moreover, individual needs vary, making expert advice crucial.
6. Other Adjunctive Treatments
In addition to medical therapies, supportive treatments such as nutritional adjustments and stress management strategies can play an important role. Ensuring the proper balance of essential vitamins and minerals, along with addressing emotional and physical stress, can help manage thyroid-related symptoms in Graves’ disease and hyperthyroidism. These approaches complement conventional treatments and promote overall well-being.
7. Selenium Supplementation
This plays an important role in thyroid health, particularly in reducing inflammation and preventing thyroid damage. Selenium supplementation is sometimes recommended to improve thyroid function and protect against oxidative stress in individuals with autoimmune thyroid disorders like Graves’ disease.
8. Long-Term Monitoring
Regardless of the treatment option, long-term monitoring of thyroid hormone levels is essential for effective management. In addition, regular check-ups help identify necessary adjustments to the treatment plan and prevent complications. Ultimately, maintaining oversight of thyroid hormone levels is vital for optimal health.
Regular blood tests and checkups help maintain a balance between treating hyperthyroidism and avoiding hypothyroidism. Through proper treatment, many patients with Graves’ disease and hyperthyroidism can achieve long-term remission or stable management of their condition.
The Connection Between Gluten and Graves’ Disease
One of the critical dietary considerations for individuals with Graves’ disease is the connection between gluten and thyroid-related autoimmune disorders, such as Graves’ and Celiac disease. Numerous studies have shown that patients with Celiac disease are at a higher risk of developing Hashimoto’s thyroiditis or Graves’ disease. Both of these are autoimmune conditions that affect the thyroid gland, with gluten playing a pivotal role in triggering the immune response. This connection is rooted in the relationship between gluten, intestinal inflammation, and the onset of autoimmune disease through a process known as molecular mimicry. In some individuals, consuming gluten can cause the immune system to attack not only the gluten but also the thyroid gland, mistaking it for a foreign invader.
Recommended Foods for People with Graves’ Disease
Following a nutrient-dense diet that supports thyroid health is critical for managing Graves’ disease. Moreover, it complements medical treatments and promotes better overall well-being.
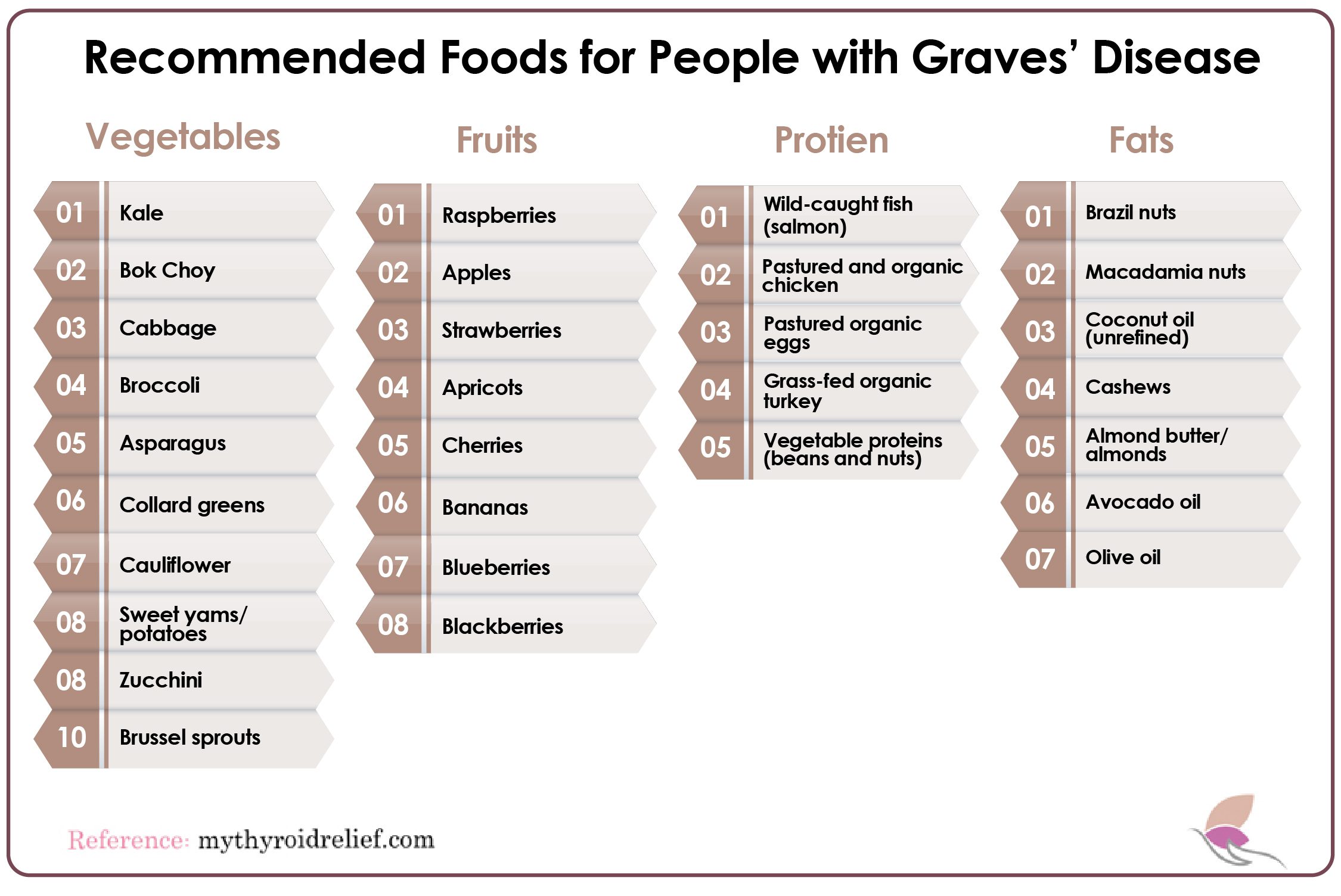
Below is a list of foods recommended for those with hyperthyroidism:
Vegetables:
- Kale
- Bok Choy
- Cabbage
- Broccoli
- Asparagus
- Collard greens
- Cauliflower
- Sweet potatoes/Yams
- Zucchini
- Brussels sprouts
Fruits:
- Raspberries
- Apples
- Strawberries
- Apricots
- Cherries
- Bananas
- Blueberries
- Blackberries
Proteins:
- Wild caught fish (Salmon)
- Pastured and organic chicken
- Pastured and organic eggs
- Grassfed organic turkey
- Vegetable proteins(beans and nuts)
Healthy Fats:
- Brazil nuts
- Macadamia nuts
- Avocado oil
- Coconut oil( Unrefined)
- Cashews
- Almond butter/Almonds
- Avocado oil
Foods to Avoid for People with Graves’ Disease
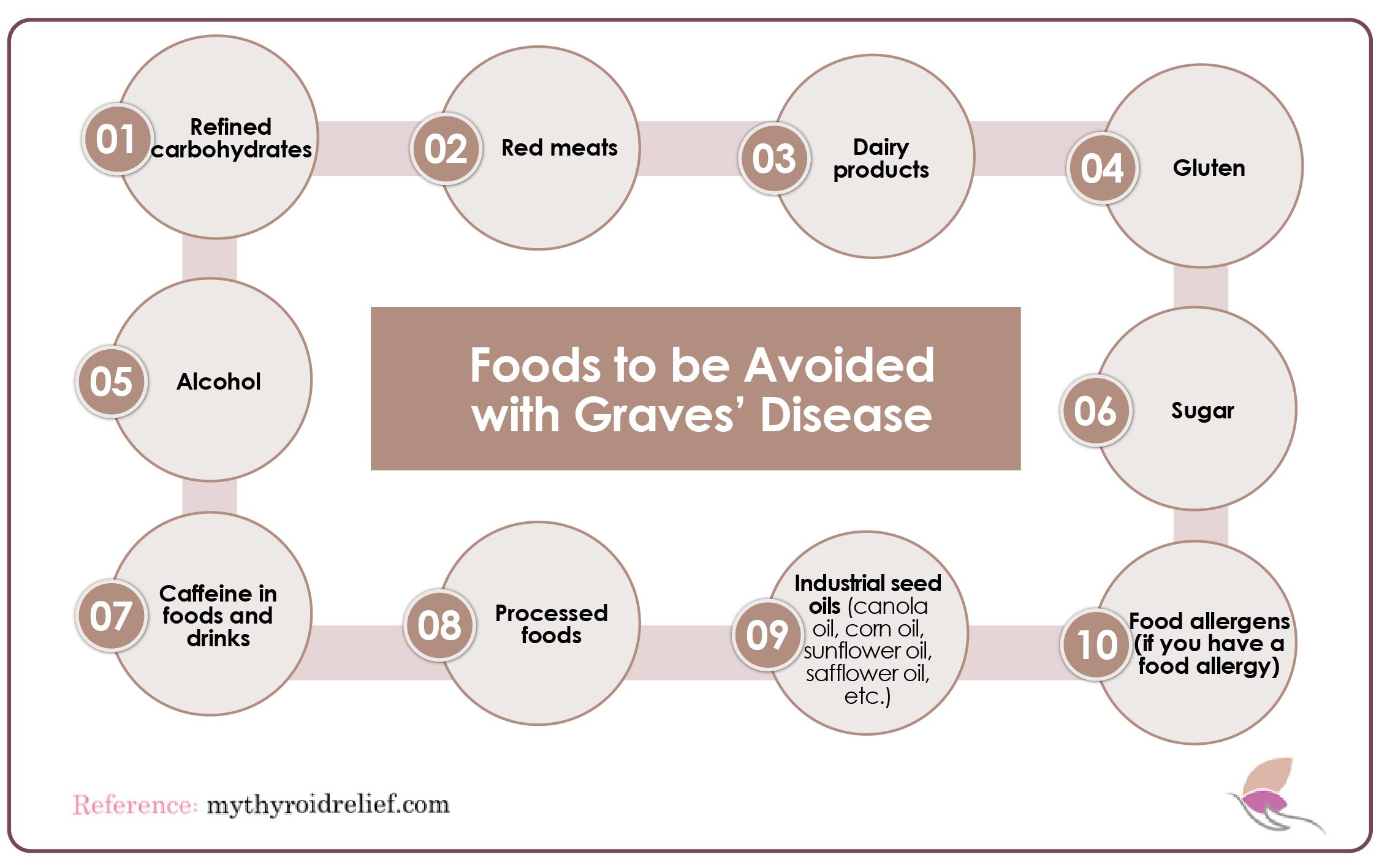
Just as important as knowing what to eat is understanding which foods to avoid, as certain items can exacerbate hyperthyroidism and trigger autoimmune responses. The following foods should be limited or eliminated from the diet:
- Refined carbohydrates
- Red meats
- Dairy products (especially if intolerant)
- Gluten
- Alcohol
- Sugar
- Caffeine in foods and drinks
- Processed foods
- Industrial seed oils (canola oil, corn oil, sunflower oil, safflower oil)
- Food allergens (if you have a food allergy)
Risk of Other Diseases with Hyperthyroidism and Grave Disease
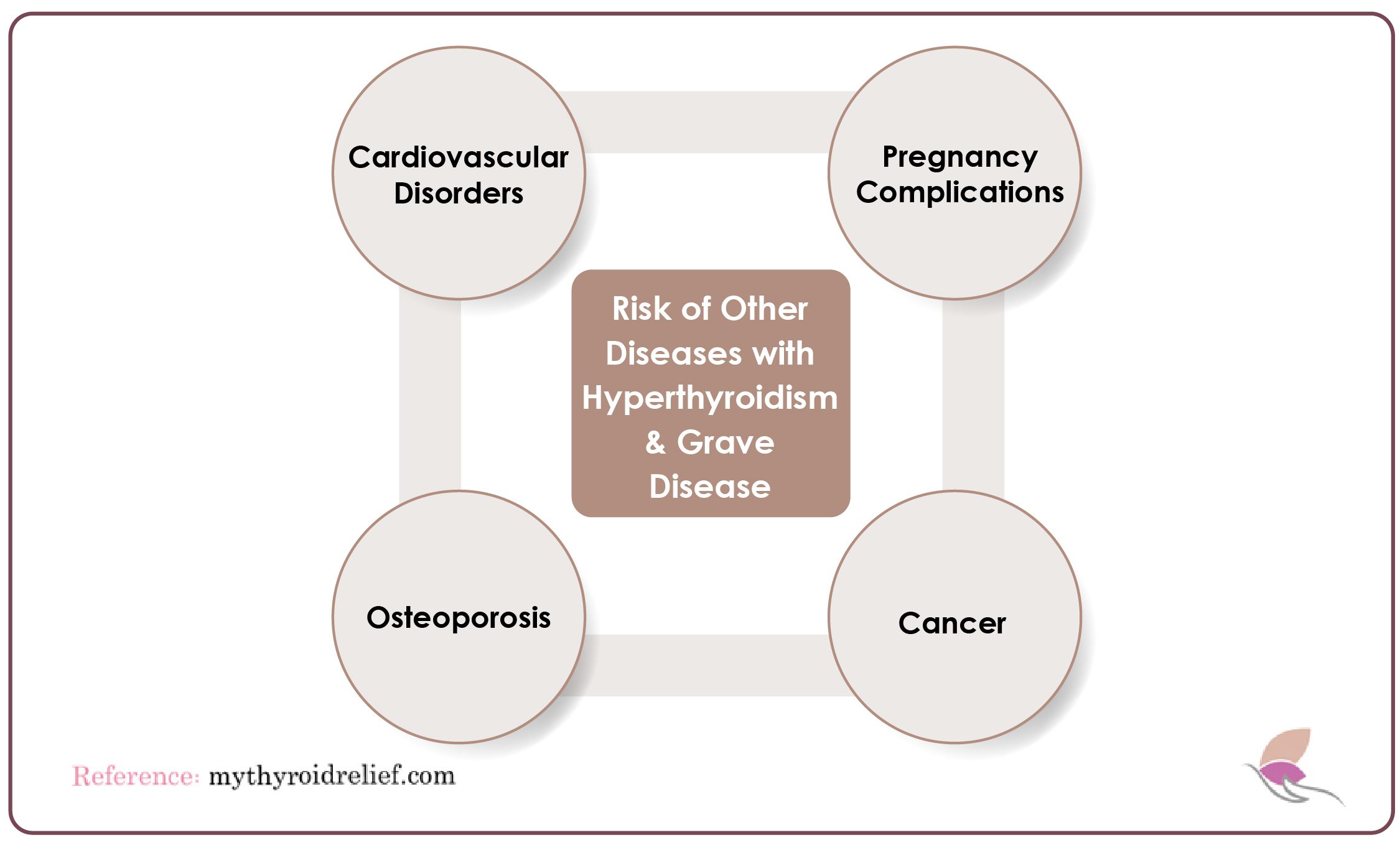
Untreated hyperthyroidism significantly raises the risk of several diseases, including:
1. Cardiovascular Disorders
Conditions affecting the heart and blood vessels, including high blood pressure, arrhythmias (irregular heartbeats), and heart failure, can increase the risk of heart attacks and strokes. These disorders are often exacerbated by the elevated metabolism and increased strain on the cardiovascular system caused by hyperthyroidism. This is especially true in cases of Graves’ disease. Addressing these cardiovascular concerns is crucial for overall health, as they can significantly impact both quality of life and treatment outcomes.
2. Pregnancy Complications
Possible complications of Graves’ disease during pregnancy include preterm birth, miscarriage, poor fetal growth, fetal thyroid dysfunction, preeclampsia, and maternal heart failure. Regular thyroid hormone tests during pregnancy are crucial for detecting irregularities early on, helping to manage potential complications for both the mother and fetus.
3. Osteoporosis
Osteoporosis is a condition characterized by weakened bones, making them fragile and more prone to fractures. It often leads to fractures in the hip, spine, and wrist, causing pain, decreased mobility, and other complications. Hyperthyroidism, particularly in individuals with Graves’ disease, can accelerate bone loss due to increased bone turnover and decreased bone density, leading to a higher risk of osteoporosis. To mitigate this risk, it is important to supplement with calcium and vitamin D, alongside engaging in regular weight-bearing exercises.
4. Cancer
The incidence of thyroid cancer is notably higher among patients with Graves’ disease—the most common cause of hyperthyroidism—compared to the general population. Recent studies suggest that the prevalence of thyroid cancer in patients with Graves’ disease ranges from 2.6% to 15%, which is notably higher than the rate in the general population. Individuals with Graves’ disease and thyroid nodules are nearly five times more likely to be diagnosed with thyroid cancer than those without nodules. A 2018 study in the Journal of Otolaryngology found that those with hyperthyroidism often have a more aggressive form of thyroid cancer, leading to a worse prognosis compared to individuals with normal thyroid function.
How Can Holistic Medicine Help Induce Remission in Graves’ Disease?
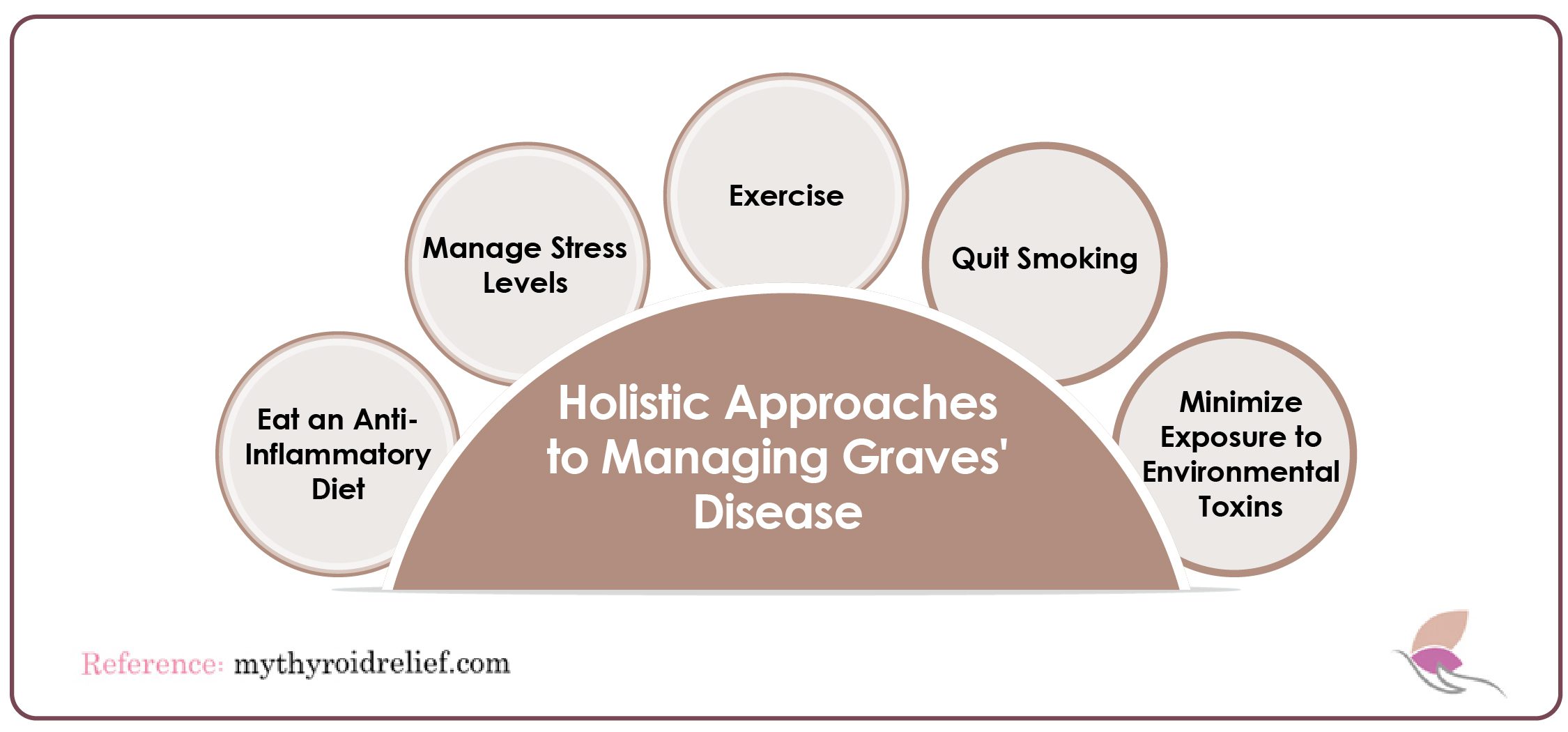
1. Manage Stress Levels
Stress significantly contributes to the exacerbation of Graves’ disease. Elevated stress levels trigger the release of adrenaline and cortisol, disrupting neurotransmitter function and worsening thyroid symptoms. Consequently, these symptoms include rapid heart rate, anxiety, and irritability. Moreover, stress can prompt the thyroid to release more hormones in hyperthyroidism and Graves’ disease, exacerbating these symptoms. To counter this, practicing stress-reduction techniques is crucial:
- Meditation and mindfulness help calm the mind and reduce cortisol levels.
- Low-impact exercises like yoga and tai chi promote relaxation without overexerting the body.
- Spending time in nature and engaging in spiritual practices like prayer can provide emotional balance.
- Massage therapy and behavioral therapy offer additional tools to manage emotional challenges associated with the disease.
Research shows that stress-induced changes in psychological, behavioral, and physiological functions can increase the risk of autoimmune diseases. Therefore, learning to manage stress is vital for managing Graves’ disease. It can help alleviate symptoms and improve long-term outcomes when combined with medical treatment.
2. Eat an Anti-Inflammatory Diet
Foods to Avoid:
- Gluten and dairy (especially conventional dairy products treated with antibiotics and hormones).
- Genetically modified (GMO) ingredients are found in many processed foods, including those with preservatives, high fructose corn syrup, and artificial chemicals.
- High-iodine foods, such as egg yolks, iodized salt, and seaweed can increase thyroid hormone levels.
Foods to Eat:
- Green juices and fresh vegetables.
- Fruits like berries, provide electrolytes and antioxidants.
- Anti-inflammatory herbs such as rosemary, basil, oregano, and parsley.
- Spices like garlic, turmeric, and ginger, enhance immune system function.
- Healthy fats (e.g., omega-3s) that possess anti-inflammatory properties and support neurotransmitter function.
- Probiotics to restore bacterial balance in the gut and combat leaky gut syndrome.
3. Exercise
Regular physical activity is an excellent way to manage stress and reduce inflammation. However, those with Graves’ disease should avoid overexertion, as excessive exercise can aggravate autoimmune symptoms. Balancing physical activity with rest, such as moderate exercises like walking or yoga, is essential for effective symptom management.
Choose exercises that are calming and help with anxiety reduction, mood enhancement, and better sleep. These exercises promote overall well-being while minimizing strain on the body, thereby helping to manage symptoms effectively. Also, they enhance flexibility and strength, ultimately contributing to improved quality of life for individuals managing their health conditions. Ideal activities include yoga, dancing, swimming, and cycling.
4. Quit Smoking
Smoking significantly increases the risk of autoimmune disorders, including Graves’ disease. Specifically, cigarette smoke contains high levels of toxins that raise inflammation and damage healthy tissues and cells. Consequently, this triggers the immune system to release T-fighter cells, potentially contributing to autoimmune flare-ups. Therefore, quitting smoking and avoiding recreational drugs is essential for reducing the risk of worsening Graves’ disease symptoms and effectively managing the condition.
5. Minimize Exposure to Environmental Toxins
Environmental toxins can also play a role in the development and worsening of autoimmune conditions like Graves’ disease. These toxins, found in common household products, beauty products, and even our food and water supply, can accumulate in the body and trigger immune responses. Reducing exposure to toxins and focusing on cleaner living can minimize inflammation and improve overall thyroid health. To reduce exposure to these harmful substances:
- Prioritize organic produce to avoid pesticide exposure.
- Opt for natural household products that are free from harmful chemicals.
- Avoid everyday items like makeup, perfumes, cookware, and furniture that contain heavy metals and toxins.
-
Minimize unnecessary medications, particularly those that disrupt hormone balance, such as birth control pills and certain antibiotics. Additionally, consider how these medications might interact with other treatments and explore alternatives when possible.
- Drink filtered water free from fluoride and chlorine. Opt for fluoride-free toothpaste to reduce fluoride intake.
Supplements and Vitamins to Help Hyperthyroidism and Grave Disease
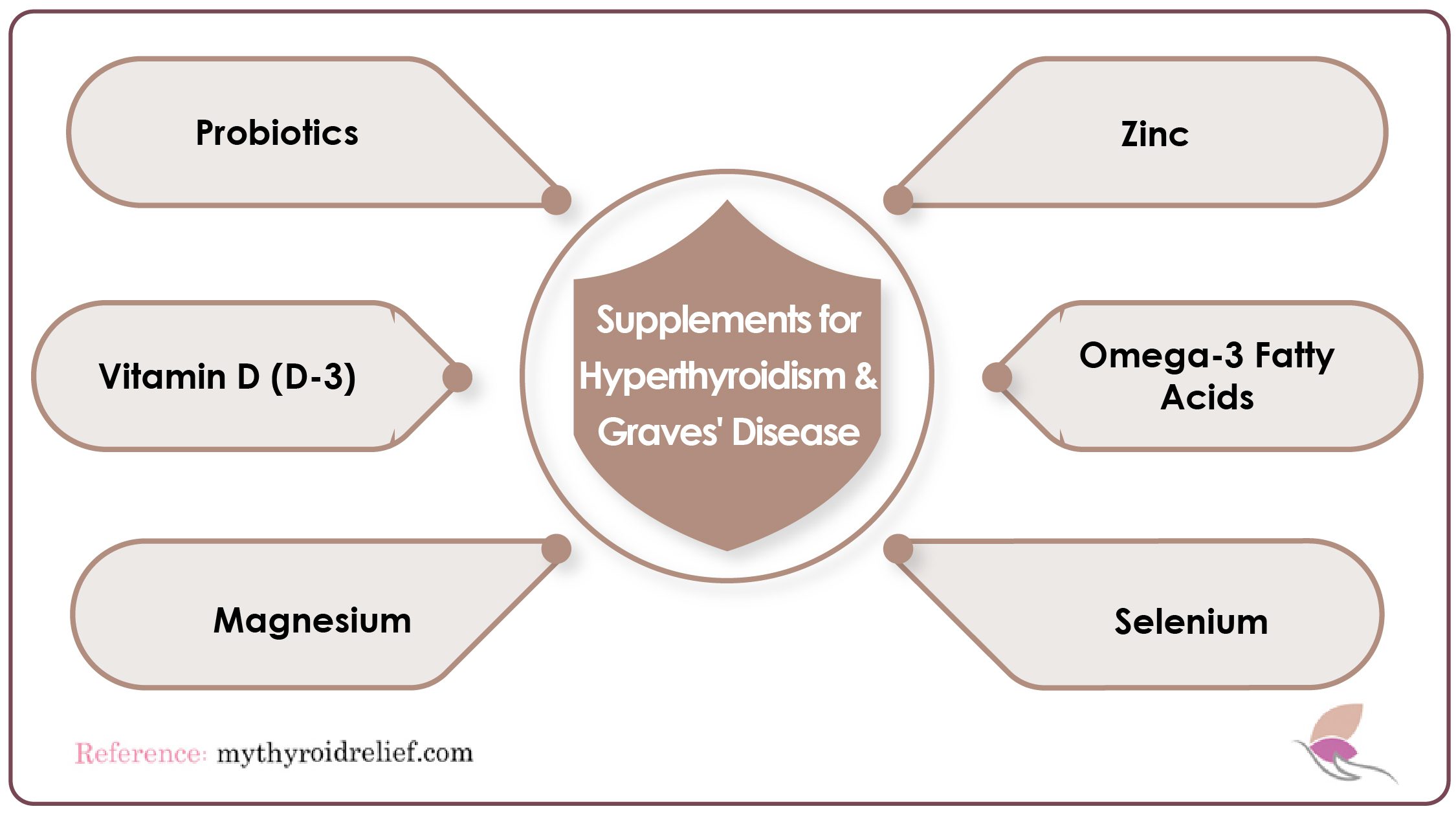
While conventional treatments such as antithyroid medications and beta-blockers are essential, incorporating natural supplements and herbs can provide additional support to your overall well-being.
If you’re looking to balance your body, calm your mind, and strengthen your immune system, here’s a comprehensive guide to supplements and herbs for managing Graves’ disease.
Herbal Supplements for Managing Hyperthyroidism and Graves’ Disease
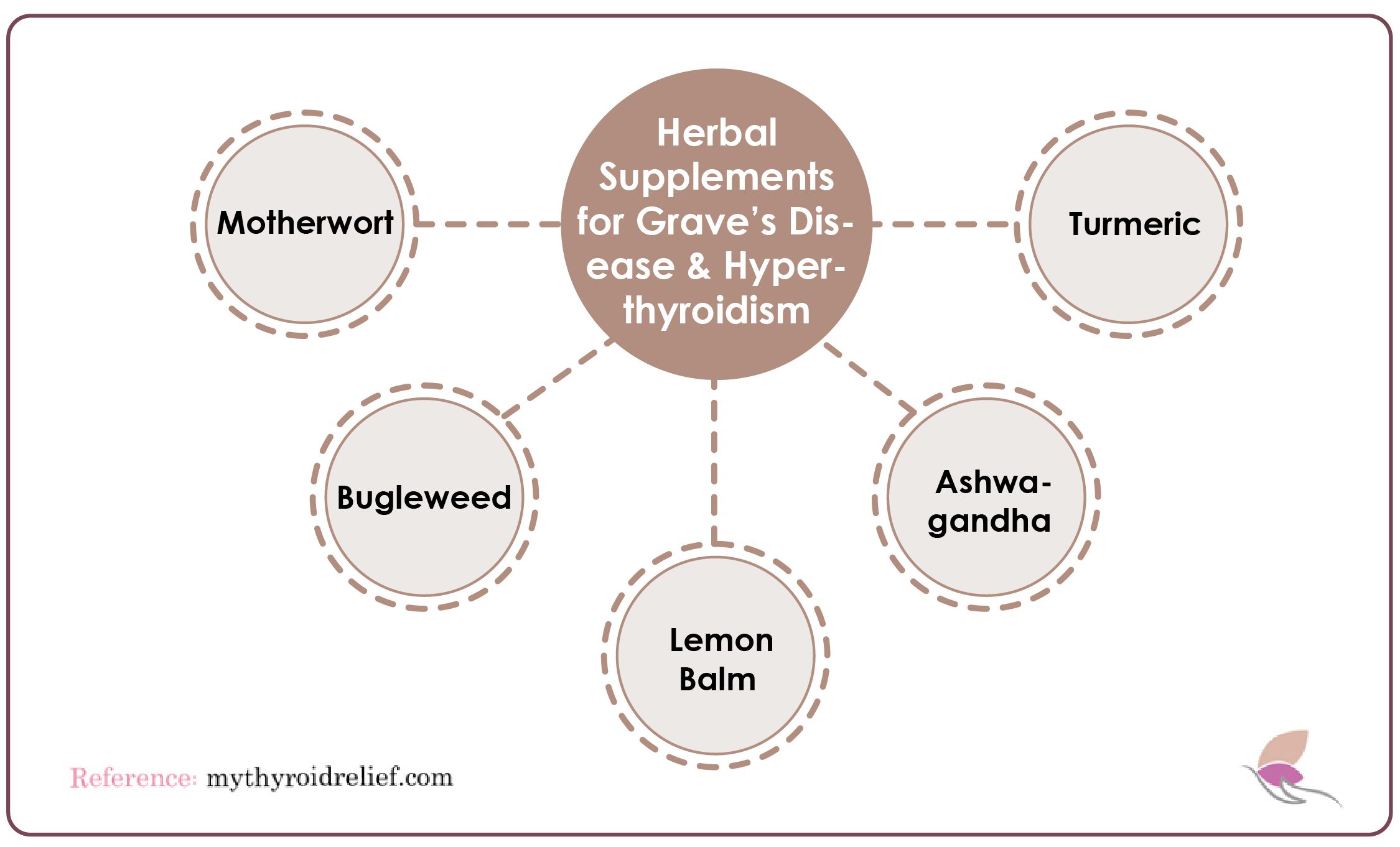
While conventional treatments are essential for managing thyroid conditions, many individuals seek complementary approaches, such as herbal supplements, which have been used for centuries to support overall health. Some of these remedies may offer natural relief for those experiencing hyperthyroidism and Graves’ disease and can complement traditional therapies to enhance well-being.
In this article, we explore several herbal supplements that may provide valuable support in managing symptoms associated with these thyroid disorders.
1. Motherwort (Leonurus cardiaca)
Motherwort, a herb with a long history in traditional medicine, is particularly known for its calming properties. It is commonly recommended for anxiety and heart palpitations, which are common symptoms of hyperthyroidism. Motherwort acts as a mild sedative, helping to soothe the nervous system and reduce feelings of restlessness and irritability. By calming both the mind and body, motherwort may alleviate psychological symptoms linked to thyroid dysfunction.
Its ability to promote relaxation can be especially beneficial for those dealing with emotional distress associated with Graves’ disease. Incorporating motherwort into a holistic approach may support emotional balance and overall well-being.
2. Bugleweed (Lycopus virginicus)
Bugleweed is another herbal remedy that has garnered attention for its potential to help manage hyperthyroidism symptoms. Traditionally used in herbal medicine, bugleweed is thought to inhibit the production of thyroid hormones, making it useful for individuals experiencing symptoms like rapid heartbeat and excessive sweating.
Bugleweed may help manage the overactivity associated with Graves’ disease by modulating thyroid function. However, individuals should consult with a healthcare professional before incorporating bugleweed into their regimen, as its effects can vary.
3. Lemon Balm (Melissa officinalis)
Lemon balm is renowned for its soothing properties and has been used for centuries to relieve stress and anxiety. For individuals with hyperthyroidism, lemon balm can help reduce emotional symptoms such as irritability and anxiety, promoting a sense of calm.
Additionally, lemon balm possesses antiviral properties, which can benefit immune health, especially those with autoimmune disorders like Graves’ disease. By alleviating stress and promoting relaxation, lemon balm may support the well-being of individuals with thyroid imbalances.
4. Ashwagandha (Withania somnifera)
Ashwagandha, an adaptogenic herb, is well-known for its ability to help the body adapt to stress. This is particularly important for individuals with hyperthyroidism, as stress can exacerbate symptoms. Ashwagandha also supports thyroid health by helping regulate the body’s response to stress. Its adaptogenic properties improve resilience and promote emotional stability, making it a valuable herb for those managing Graves’ disease.
5. Turmeric (Curcuma longa)
Due to its active compound, curcumin, turmeric possesses potent anti-inflammatory and antioxidant properties. Chronic inflammation is a hallmark of autoimmune conditions like Graves’ disease, making turmeric particularly beneficial. Including turmeric in the diet or as a supplement can reduce inflammation and support overall health. Additionally, turmeric promotes liver function, which is essential for hormone metabolism, further supporting thyroid health.
Conclusion
In conclusion, managing Graves’ disease and hyperthyroidism effectively requires a comprehensive approach that combines medical treatments, dietary modifications, and regular monitoring. Anti-thyroid medications, beta-blockers, and surgical options like thyroidectomy can help regulate hormone levels and alleviate symptoms, depending on the severity of the condition.
Adopting a nutrient-rich, anti-inflammatory diet is equally crucial. Foods such as cruciferous vegetables, berries, and healthy fats can support thyroid function, while avoiding triggers like gluten and high-iodine foods may help minimize autoimmune flare-ups and improve overall quality of life.
Routine check-ups and blood tests are essential for tracking thyroid hormone levels and ensuring that treatments remain effective. An individualized approach is vital, as each patient may respond differently to interventions.
With the right combination of medical care and lifestyle changes, individuals with Graves’ disease can significantly reduce the risk of complications such as thyroid storm and cardiovascular issues. This holistic approach promotes long-term health, balance, and well-being.
References
https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease
https://www.mayoclinic.org/diseases-conditions/graves-disease/symptoms-causes/syc-20356240
https://emedicine.medscape.com/article/120619-overview
https://medlineplus.gov/hyperthyroidism.html
Understanding the nuances of Graves’ disease and hyperthyroidism is crucial for effective management and improving quality of life. This post empowers patients to take an active role in their healthcare journey by providing important facts and insights. It’s essential for patients to be well-informed about their condition, treatment options, and potential complications. Thank you for sharing these important facts—it’s sure to make a positive difference in the lives of many patients.