Dysautonomia refers to a group of disorders that impair the autonomic nervous system (ANS), leading to malfunctions that disrupt the regulation of vital bodily functions. The ANS controls automatic processes such as heart rate, blood pressure, digestion, and body temperature. When the ANS malfunctions, symptoms can range from mild dizziness to severe complications, including fainting, chronic fatigue, and difficulty regulating blood pressure.
Hashimoto’s disease, an autoimmune condition targeting the thyroid gland, has increasingly been linked to dysautonomia. The two conditions share common triggers and can overlap in their effects on the body, leading to complications that make diagnosis and treatment more challenging. This article explores dysautonomia, its connection to Hashimoto’s disease, and the common forms of dysautonomia that affect individuals. It also examines how early diagnosis and management can significantly improve quality of life for those managing these interconnected conditions.
Types of Dysautonomia
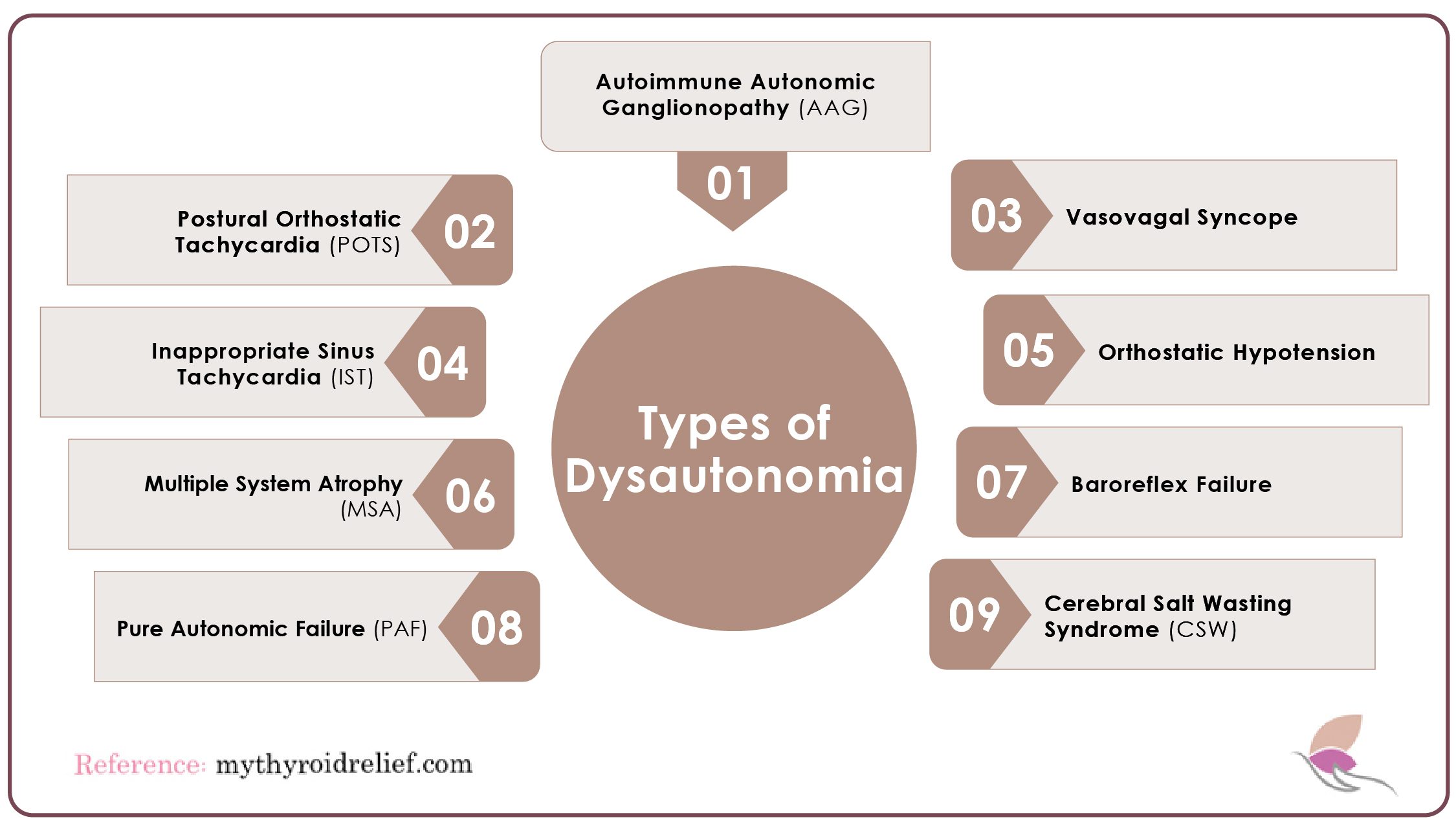
There are over 15 different types of dysautonomia, each presenting distinct symptoms and challenges. Below are some of the most common forms:
1. Postural Orthostatic Tachycardia Syndrome (POTS)
POTS is the most frequently diagnosed form of dysautonomia, affecting how blood circulates throughout the body. Individuals with POTS experience a rapid increase in heart rate and a drop in blood pressure when standing, making it difficult to stay upright. Symptoms may include dizziness, fainting, and fatigue. POTS primarily affects women and is most commonly diagnosed in adults aged 15 to 50. Approximately 1 to 3 per 100,000 people are estimated to have this condition.
2. Vasovagal Syncope
This form of dysautonomia causes fainting due to a sudden drop in blood pressure, often triggered by stress, pain, or even the sight of blood. While it is not life-threatening, vasovagal syncope can be dangerous if a fainting episode occurs while driving or operating machinery. Symptoms such as dizziness, nausea, and sweating typically precede fainting, with recovery occurring within a few minutes.
3. Orthostatic Hypotension
Orthostatic hypotension occurs when blood pressure drops significantly upon standing, causing dizziness or nausea. It is commonly seen in older adults or those with conditions like diabetes and Parkinson’s disease. Treatment often involves increasing fluid intake, adjusting medications, and making lifestyle changes to avoid prolonged periods of standing or sitting.
4. Inappropriate Sinus Tachycardia (IST)
IST is characterized by an abnormally fast heart rate at rest, without any clear physical or emotional trigger. Symptoms include palpitations, shortness of breath, and chest pain. Although not typically life-threatening, IST can significantly affect daily activities and may require treatment to manage heart rate and associated symptoms.
5. Autoimmune Autonomic Ganglionopathy (AAG)
AAG is an autoimmune disorder where the body’s immune system attacks the autonomic nervous system, disrupting functions like heart rate and blood pressure control. It is a rare condition that is difficult to diagnose because its symptoms resemble those of other disorders. Although there is no cure, treatments focus on managing symptoms and improving the quality of life.
6. Baroreflex Failure
The baroreflex system helps regulate blood pressure. When it fails, patients may experience dangerous fluctuations in blood pressure, which can be life-threatening. Causes of baroreflex failure include heart disease and certain types of hypertension. Treatment typically involves medications that help stabilize blood pressure.
7. Multiple System Atrophy (MSA)
MSA is a neurodegenerative disorder that affects both the central and peripheral nervous systems. It causes symptoms similar to Parkinson’s disease, along with autonomic dysfunction like blood pressure problems and urinary issues. Although MSA is a rare and progressive condition, treatments can help manage symptoms, but it is often fatal within 10 years of diagnosis.
8. Pure Autonomic Failure (PAF)
PAF results from the gradual failure of the autonomic nervous system, leading to issues such as impaired blood pressure regulation, heart rate control, and bladder function. Primarily affecting older adults, PAF can progress into multiple system atrophy. Although there is no cure, treatments can help manage symptoms and enhance the quality of life.
9. Cerebral Salt Wasting Syndrome (CSW)
CSW is a rare condition that causes the body to lose excessive amounts of salt, leading to dehydration. It is often associated with brain injuries or surgeries and can be life-threatening if not treated. Symptoms include headaches, nausea, vomiting, and seizures. Treatment involves replenishing lost salt and fluids through intravenous or oral means.
Symptoms of Dysautonomia
Symptoms of dysautonomia can vary widely among individuals, but several common signs are frequently reported. Recognizing these symptoms is essential for early diagnosis and effective management.
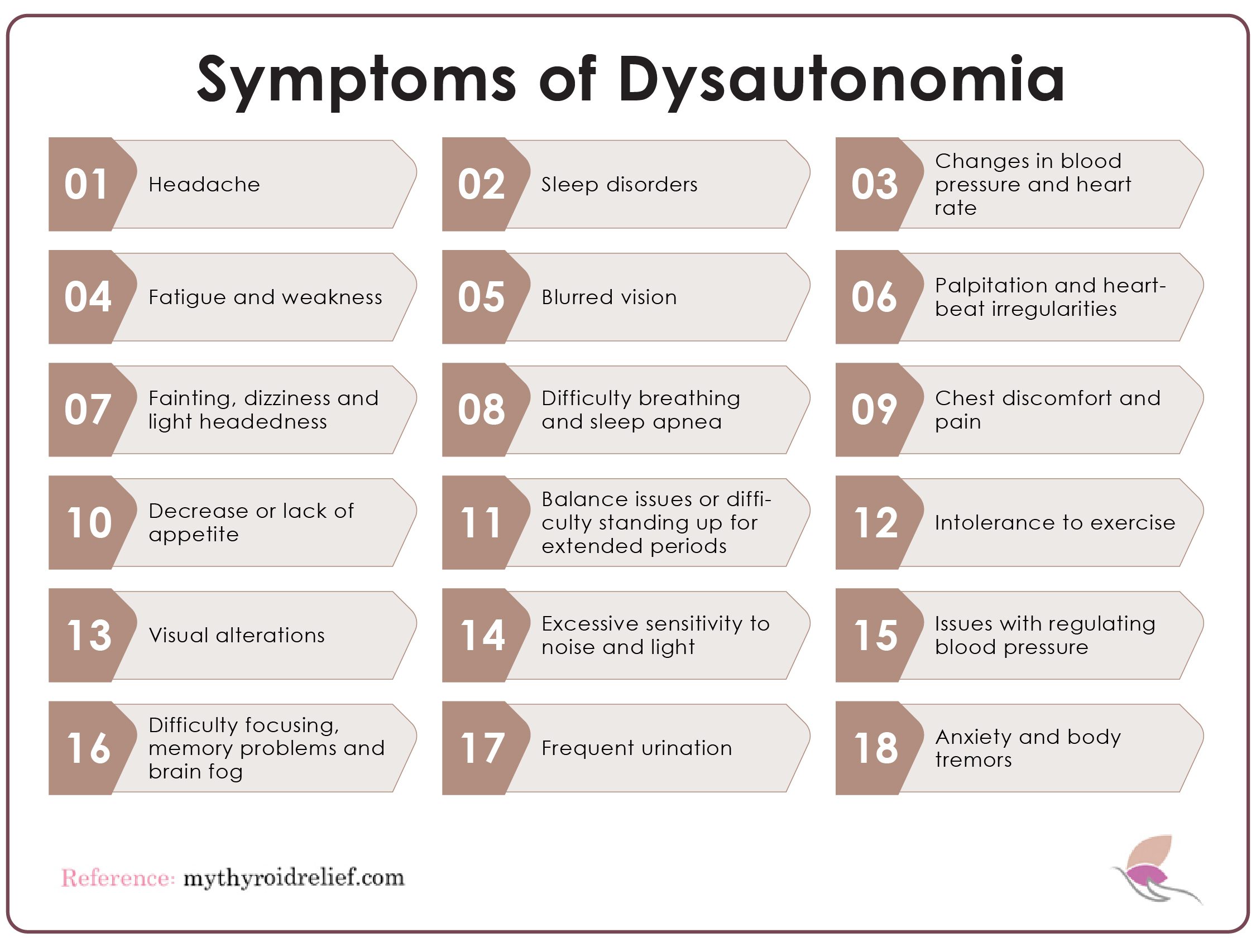
Below are some primary symptoms associated with dysautonomia:
1. Headache
2. Sleep disorders
3. Changes in blood pressure and heart rate
4. Fatigue and weakness
5. Blurred vision
6. Palpitation and heartbeat irregularities
7. Fainting, dizziness and light headedness
8. Difficulty breathing and sleep apnea
9. Chest discomfort and pain
10.Decrease or lack of appetite
11.Balance issues or difficulty standing up for extended periods
12. Intolerance to exercise
13.Visual alterations
14. Excessive sensitivity to noise and light
15. Issues with regulating blood pressure
16. Difficulty focusing, memory problems and brain fog
17. Frequent urination
18. Anxiety and body tremors
What Are Some Possible Causes of Dysautonomia?
Dysautonomia can result from a variety of conditions that damage the autonomic nervous system (ANS), disrupting the regulation of essential functions such as heart rate, blood pressure, and digestion.
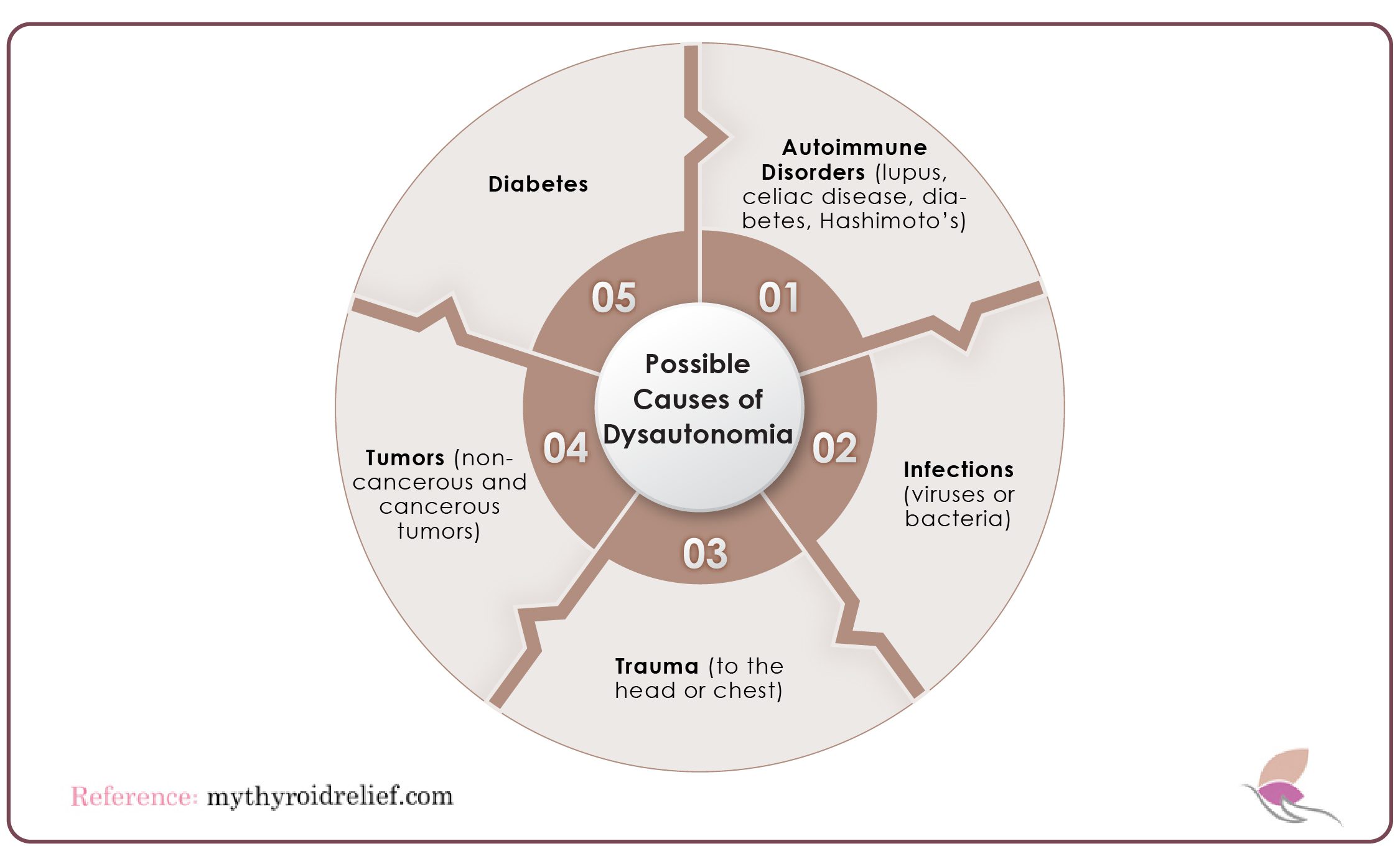
Here are some potential causes:
- Autoimmune Disorders: Diseases like lupus, celiac disease, diabetes, and Hashimoto’s thyroiditis can lead to dysfunction of the ANS. In these conditions, the immune system mistakenly attacks healthy tissues, including nerve cells that control autonomic functions. Over time, this damage impairs the regulation of body functions, leading to dysautonomia symptoms.
- Infections: Viral and bacterial infections, such as Epstein-Barr virus or Lyme disease, can cause inflammation of the nerves controlling the ANS. This inflammation may disrupt normal signals, resulting in issues like orthostatic intolerance, where standing causes dizziness or fainting. In some cases, the infection may directly damage nerve tissues, leading to long-term complications.
- Trauma: Physical injuries, especially to the head, neck, or chest, can cause damage to the ANS. Traumatic brain injuries, whiplash, or chest trauma may impair autonomic functions. For example, a blow to the head can affect the brain’s ability to regulate blood pressure or heart rate.
- Tumors: Benign (non-cancerous) or malignant (cancerous) tumors can press on or invade areas where autonomic nerves are located. This compression can disrupt nerve signaling, causing symptoms like irregular blood pressure or abnormal heart rates. Tumors in the brain, spinal cord, or near vital organs may directly impact the ANS.
- Diabetes: Chronic high blood sugar levels can damage the small nerves controlling autonomic functions, a condition known as diabetic neuropathy. This often affects the heart, bladder, and digestive tract. Diabetic dysautonomia may lead to difficulties in regulating blood pressure or digestive issues like gastroparesis.
How is Dysautonomia Diagnosed?
Dysautonomia is challenging to diagnose because there is no single test to detect it. Instead, healthcare professionals rely on a combination of medical history, reported symptoms, and physical examinations. Your doctor will likely inquire about your family history, the medications you are taking, and other relevant medical details. A physical exam is conducted to check for signs such as low blood pressure, rapid heart rate, or abnormal sweating. Tests may be ordered to rule out other conditions, such as thyroid problems or anemia.
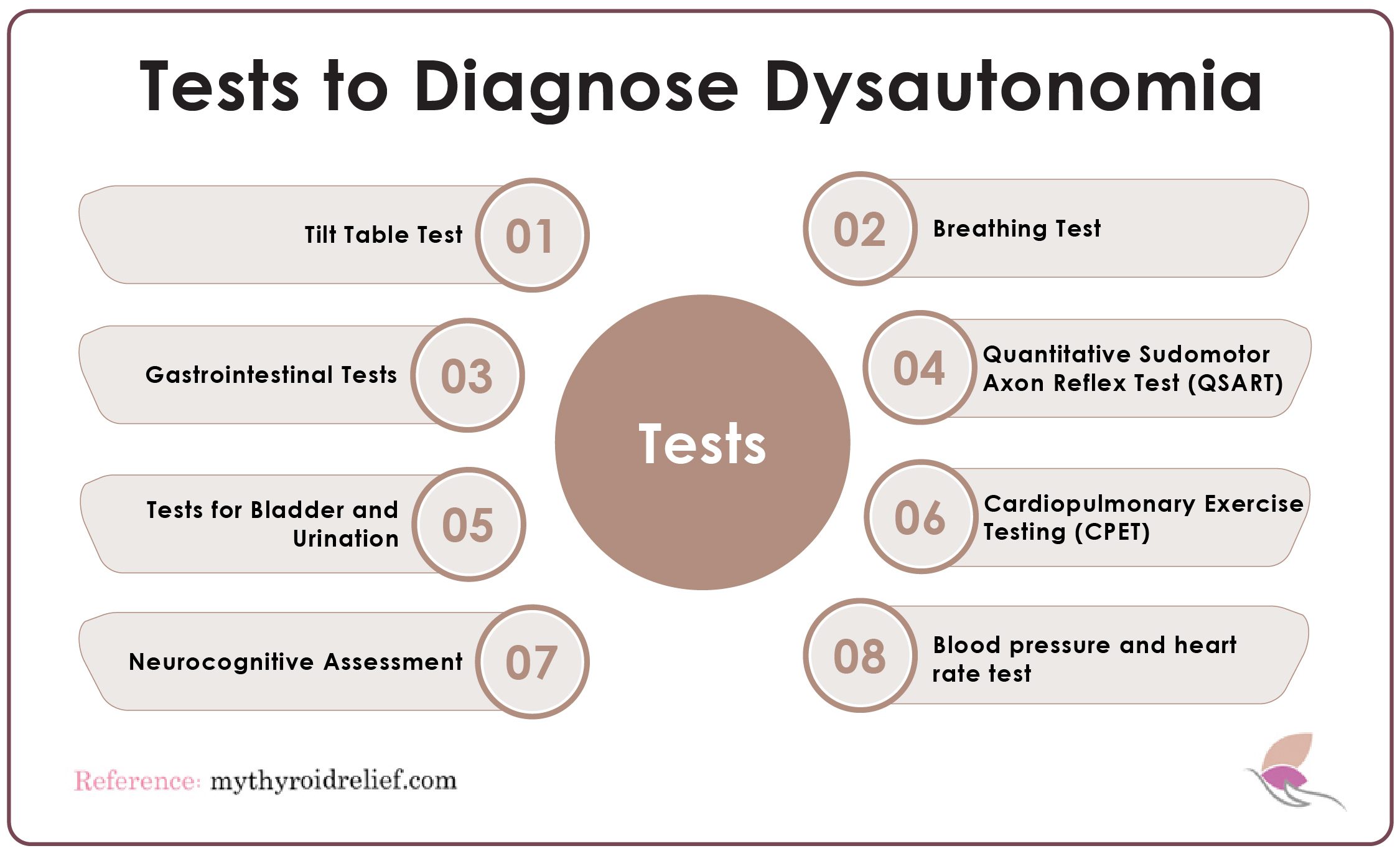
Common tests for diagnosing dysautonomia include:
1. Tilt Table Test
This test evaluates how your autonomic nervous system responds to changes in position. During the test, you lie on a table that tilts from horizontal to vertical while your heart rate and blood pressure are monitored. It helps diagnose conditions such as syncope, hypotension, or orthostatic hypotension.
2. Breathing Test
Breathing tests, such as spirometry, assess lung function by measuring how much air you can inhale and exhale. While typically used for respiratory conditions like asthma or COPD, these tests can also help identify autonomic dysfunction affecting breathing.
3. Gastrointestinal Tests
Dysautonomia often affects the gastrointestinal (GI) system, slowing down digestion. Tests like gastric emptying studies, breath tests, and endoscopies help assess how food and liquids pass through the GI tract. These tests are important because slow transit times can indicate autonomic issues.
4. Quantitative Sudomotor Axon Reflex Test (QSART)
The Quantitative Sudomotor Axon Reflex Test (QSART) measures how well the autonomic nervous system controls sweating by applying a small electrical current to areas like the forearm and foot. This test is crucial for diagnosing conditions like diabetic neuropathy.
5. Tests for Bladder and Urination
Some individuals with dysautonomia experience bladder dysfunction. Tests such as urodynamic studies and ultrasounds assess bladder function, checking for abnormalities like bladder retention or irregular voiding patterns, which can be linked to autonomic dysfunction.
6. Cardiopulmonary Exercise Testing (CPET)
This test measures heart and lung performance during exercise. The patient exercises on a stationary bike while wearing a heart rate monitor and breathing into a mask that tracks oxygen and carbon dioxide levels. CPET evaluates how dysautonomia affects physical activity and helps monitor treatment progress.
7. Neurocognitive Assessment
A neurocognitive assessment evaluates cognitive functions such as memory, attention, and language. Doctors often use it to identify cognitive impairments caused by autonomic dysfunction. Various tests are conducted on a computer, assessing brain function and identifying issues linked to dysautonomia.
Treatments of Dysautonomia
Although dysautonomia has no definitive cure, several treatments can help manage its wide range of symptoms.

- Medication: Although dysautonomia has no definitive cure, several medications can help manage its wide range of symptoms. Doctors often prescribe medications to regulate blood pressure and heart rate, both of which can become unstable in individuals with dysautonomia. Beta-blockers or vasoconstrictors may be used to control heart rate and improve blood flow.
- Mindfulness Techniques: Practices such as yoga, meditation, and deep breathing exercises are beneficial for managing both the physical and emotional stress associated with dysautonomia. These techniques promote relaxation, help reduce anxiety, and improve overall mental well-being. Since dysautonomia often exacerbates stress, integrating mindfulness into daily routines can significantly improve symptom management.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals challenge negative thought patterns and develop healthier mental habits. This therapy is particularly valuable for dysautonomia patients who may also experience anxiety, depression, or other mental health challenges. By encouraging positive behavior changes and improved coping strategies, CBT helps patients manage the emotional burden of chronic illness.
- Cannabidiol (CBD): CBD, a non-psychoactive compound from the cannabis plant, has been reported to alleviate common dysautonomia symptoms such as pain, anxiety, and sleep disturbances. It is available in oils, capsules, and tinctures, but it’s important to consult a healthcare provider before use to ensure it’s safe and appropriate for your condition.
What is the connection between Dysautonomia and Hashimoto’s disease?
Recent studies highlight a link between Hashimoto’s thyroiditis, an autoimmune disorder affecting the thyroid gland, and dysautonomia, which impacts the autonomic nervous system (ANS). Hashimoto’s disease causes hypothyroidism, leading to hormonal imbalances that can disrupt the ANS, resulting in secondary dysautonomia. Individuals with Hashimoto’s disease are more likely to develop dysautonomia because both conditions share common autoimmune triggers that cause the immune system to attack healthy tissues.
Immune attacks on the thyroid gland can lead to widespread inflammation, affecting the ANS and disrupting vital functions like heart rate, blood pressure, and digestion. Overlapping symptoms, such as fatigue, dizziness, and brain fog, can complicate diagnosis, making it essential for healthcare providers to consider dysautonomia in Hashimoto’s patients. Recognizing this connection allows for earlier diagnosis and treatment, preventing complications and improving quality of life.
Advanced medical centers, such as Schofield’s, have developed improved screening methods for both conditions, ensuring earlier and more accurate diagnoses. Proper treatment helps mitigate symptoms and ensures better health outcomes for affected individuals.
Managing Dysautonomia and Hashimoto’s Disease
Managing dysautonomia associated with Hashimoto’s disease requires a comprehensive approach that addresses both conditions effectively. Here are key steps to consider:
- Thyroid Hormone Replacement: Since Hashimoto’s disease causes hypothyroidism, thyroid hormone replacement therapy is the first priority. This helps regulate thyroid hormone levels and reduces symptoms such as fatigue, brain fog, and muscle weakness. By managing hypothyroidism, the strain on the autonomic nervous system is alleviated.
- Medications for Dysautonomia: Specific medications may be needed to manage dysautonomia symptoms. Beta-blockers may be prescribed to control heart rate, or fludrocortisone to help regulate blood pressure. These medications aim to stabilize blood pressure and prevent dizziness or fainting, which are common in dysautonomia.
- Lifestyle Adjustments: Making simple changes to your daily routine can significantly reduce symptoms. Increasing salt and water intake helps elevate blood pressure, while avoiding triggers like extreme heat, prolonged standing, and dehydration can minimize autonomic dysfunction. Regular, low-impact exercises such as yoga or walking can also improve circulation and overall health.
- Dietary Considerations: A healthy, balanced diet is essential. Avoiding caffeine, alcohol, and excessive sugar can prevent symptom flare-ups. A diet rich in whole grains, vegetables, and lean proteins supports both thyroid and autonomic function.
- Ongoing Monitoring: Regular check-ups with healthcare providers are crucial to effectively managing both conditions. Adjustments to medications or lifestyle strategies may be necessary as symptoms evolve. Ongoing monitoring ensures that the treatment plan is tailored to the individual’s specific needs.
References
- https://my.clevelandclinic.org/health/diseases/6004-dysautonomia
- https://www.aurorahealthcare.org/services/neuroscience/neurology/neurological-conditions/dysautonomia
- https://thedysautonomiaproject.org/identifying-dysautonomia/
- https://www.medicalnewstoday.com/articles/76785
- https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
It’s eye-opening to see how these conditions overlap and impact daily life. Thanks for shedding light on such an important topic!