Table of Contents
Toggle
The thyroid gland regulates the body’s metabolism, energy levels, and brain functioning. It plays a vital role in the bioavailability of the sex hormones: estrogen, testosterone, and progesterone.
If you are a hypothyroid patient, then there’s a chance you’re already familiar with some of the symptoms, like weight gain, fatigue, memory, and mental concentration problems.
Menopause and its impact on your body
When a woman hasn’t had a period for 12 months, menopause is thought to have started.
In some women, menopause may be characterized by uncomfortable symptoms, including weight gain and hot flashes. However, most women do not require medical treatment for menopause.
At what age does menopause begin?
Menopause usually begins between 45 and 55 but may develop a little before or after this age range. Menstrual periods are usually irregular during perimenopause. You may see your periods late or, in some cases, may skip one or more periods entirely. Your menstrual flow may also lighten or become heavier. Post-menopause is the period after menopause has taken place.
In most cases, menopause symptoms start at least four years before a woman’s last period. However, symptoms may persist until at least four years after the woman’s last period.
Some women may experience the symptoms of menopause for at least a decade, leading to menopause itself. According to the NHS, 1 in 10 women experiences the symptoms of menopause for up to 12 years after their last period.
Fifty-one years is the median age for menopause. However, Latina and Black women may experience it two years earlier. Therefore, there is a need for more studies to understand the precise onset of menopause for women of color.
You see, it isn’t so difficult to determine when your menopause will begin. Several factors can help you determine when exactly yours will start. Ovary health and genetics are good examples. In addition, perimenopause is the period before menopause. During perimenopause, your hormones change in preparation for menopause.
Perimenopause can last for a few months to a couple of years. In most cases, perimenopause begins after the mid-40s. In some women, perimenopause does not even occur. They just enter into menopause.
At least one percent of women get into menopause before age 40. This condition is called primary ovarian insufficiency or premature menopause. Studies have also shown that over five percent of women may enter menopause between 40 and 45. This is known as early menopause.
The connection between menopause and hypothyroidism
I’m sure most of us would agree that menopause is an essential transition in a woman’s life that brings about profound changes on physical and emotional levels. Perimenopause, the timeline that leads to menopause, can temporarily shift the body’s balance with the hormones recalibrating and readjusting to a new set of demands.
Since it is no longer subjected to the rigors of childbearing, the body uniquely conserves its energy and slows estrogen and progesterone production. Progesterone is the first hormone to decline in menopause, producing a disbalance hormonal with estrogen and can cause a risk of developing osteoporosis, problems with weight gain, and cardiovascular disease.
Some practitioners and researchers believe that estrogen dominance contributes to decreased thyroid function. In addition, the pairing of estrogen with low progesterone levels, a situation typical for most perimenopausal women, may impede thyroid hormone action resulting in the symptoms of hypothyroidism, even when thyroid hormone blood tests appear normal on laboratory results.
Estrogen dominance plays a significant role in thyroid problems during perimenopause and menopause. There are several factors that one should consider during perimenopause and menopause. First, our body systems are interconnected. A disease or a health condition may start in some other part of the body and not necessarily the organ or tissue exhibiting the condition. The thyroid isn’t exempted. So, a thyroid condition may originate in another part of the body.

Untreated hypothyroidism can trigger premature perimenopause.
How does untreated hypothyroidism trigger menopause? That’s what we will focus on in this section.
You see, estrogen production becomes erratic with the onset of the menopause transition. The duration of perimenopause varies from one woman to the other, sometimes extending for months or years. Perimenopause is characterized by an array of symptoms, such as night sweats and changes in the character and frequency of the menstrual cycle.
Alterations in hormone levels, especially estrogen, contribute immensely to mood swings, waves of hot flashes, and foggy thinking. There is also the discomfort of vaginal dryness and sleep disruptions.
The fluctuations in estrogen that occur during the transition to menopause influence thyroid function because estrogen regulates thyroid-binding globulin (TBG), the hormone-binding protein. More TBG is produced by your liver when estrogen levels are high.
Thus, the blood levels of T3 and T4 temporarily drop until the thyroid gland is stimulated to produce more. On the other hand, when estrogen levels drop temporarily, for instance, during a skipped menstrual cycle, TBG falls to very low levels, followed by a temporary increase in the amount of ‘free’ T3 and T4. These alterations in thyroid hormones are not well understood but may influence some perimenopause symptoms.
For some women, irritability and weight gain may be an indicator of underlying thyroid issues. The question comes: how does a woman if her perimenopause symptoms are due to an untreated hypothyroid condition?
To answer that question, we have to understand what happens when the thyroid secretes very little T3 and T4 hormones. Hypothyroidism is a good place to start. Why? Because the symptoms of hypothyroidism often overlap with the changes that take place in female midlife.
Thyroid levels
When your thyroid levels fall to very low levels, most bodily functions slow. The affected person fatigues more readily. The skin becomes dry and the affected person may develop constipation. A woman may observe that she’s feeling depressed more often, her menstrual cycle changes drastically, and her memory stalls. She may also feel cold every time.
Hypothyroidism is associated with autoimmunity most of the time. Hashimoto’s disease is the most common cause of hypothyroidism. In Hashimoto’s disease, your thyroid gland is attacked by your immune system. You may have goiter (an enlarged thyroid), which may cause a swelling in the front of your neck.
Your risk of hashimoto’s disease is higher if you have an underlying autoimmune condition, or there’s a history of hashimoto’s in your family.
Attributing the symptoms of hypothyroidism to perimenopause without proper testing may result in its underdiagnosis.
It is important to discuss your concerns with your healthcare provider since untreated hypothyroidism may contribute to the risk of heart disease, elevated blood pressure, cholesterol, and other conditions.

Lower levels of reproductive hormones affect the thyroid
I’ve discovered a couple of factors one should consider at this transition point.
During perimenopause, the aging ovaries start producing unpredictable estrogen and progesterone levels.
This is undoubtedly an irregular hormonal activity that is potentially confusing to the body and may result in mood swings, erratic periods, and hot flashes. Breast tenderness, vaginal dryness, fatigue, night sweats, forgetfulness, and difficulty sleeping are common during menopause. In addition, fluctuating hormonal symptoms are experienced by many women in the decade that lead to actual menopause.
It is important to note that these symptoms are all associated with lower estrogen levels. You see, estrogen levels decrease drastically during the menopausal transition. As a result, the menstrual cycles become farther apart, longer, and unpredictable.
Thyroid function is also affected by varying estrogen levels. Estrogen affects the thyroid glands’ ability to produce adequate triiodothyronine (T3) and thyroxine (T4) to meet the body’s needs. The pituitary gland responds by releasing plenty of TSH into the general circulation (the bloodstream) to stimulate the Thyroid.
Remember: the transition to menopause is quite unpredictable, so a woman may have low estrogen levels and very high amounts on other days. Too much estrogen affects thyroid health. High blood levels of estrogen signal increased production of thyroid-binding globulin (TBG) by the liver. It binds to thyroid hormones and reduces the amount of T4 and T3 available for cell utilization. In response, the thyroid gland increases production to compensate for the deficit.
Studies and Researchs in menopause and thyroid issues
Scientists and healthcare professionals have debated the relationship between menopause and hypothyroidism for quite a while. The reason for this is that thyroid function isn’t stable. Instead, it dwindles gradually as we get older. What’s more, less iodine gets into the general circulation (bloodstream) as we age; consequently, the thyroid gland produces low levels of T4 and problems converting to FT4 and FT3 in the body.
A study [4] published in the journal Gynecological Endocrinology shows that suboptimal thyroid function slows the conversion of thyroxine into triiodothyronine. The result is a domino effect that begins with the liver and gallbladder and then returns to the thyroid gland. No doubt, it is a vicious circle.
Researchers have focused on the relationship between hypothyroidism and the transition to menopause.
TSH and Menopause
High TSH is a sign of an underactive thyroid since the pituitary gland releases the TSH into the bloodstream to stimulate the production and release of more T4 and T3 from the thyroid gland. In addition, changes in estrogen levels released by the ovaries during menopause can affect blood levels of TSH and thyroid hormones.
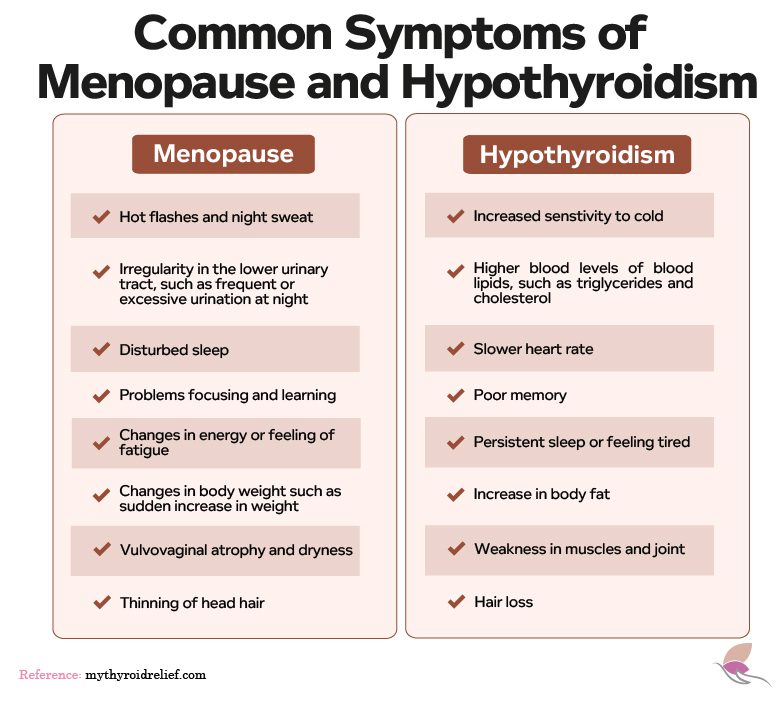
In some cases, differentiating the symptoms of menopause and hypothyroidism can be very tricky since they are similar. For example, forgetfulness, moodiness, depression, weight changes, and irregular menstrual cycles are linked to menopause and hypothyroidism.
It is worth mentioning that hyperthyroidism and menopause may also share a couple of symptoms, including heart palpitations, sleep disturbances, hot flashes, and heat intolerance.
Hyperthyroidism, hypothyroidism, and other thyroid conditions can increase your risk of menopause-related complications, such as heart disease, insomnia, weight gain, and urinary tract infection.
Complications in menopause with hypothyroidism
Thyroid conditions can increase your risk of complications of menopause. Osteoporosis is one of the most common complications of menopause. Studies have shown that hypothyroidism can cause a drastic reduction in bone density [6]. Women with low body fat (especially Caucasians) risk osteoporosis the most.
A high risk of cardiovascular disease is another complication of menopause. In addition, low thyroid hormone levels can also increase the risk of heart conditions [7].
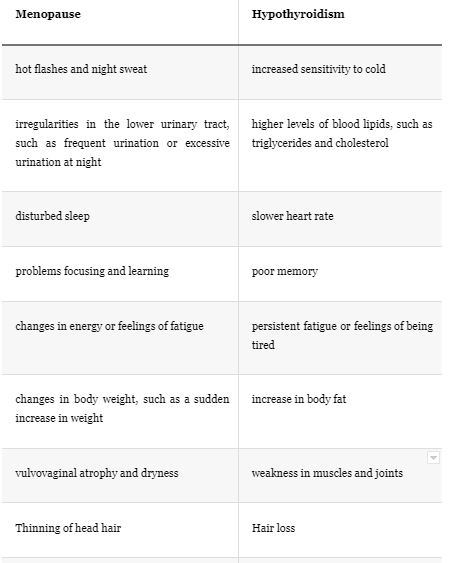
How symptoms of hypothyroidism overlap the symptoms of menopause
Signs are commonly seen in menopause and hypothyroidism
Weight problems during menopause
Hormonal changes and weight gain occur even as women switch into menopause.
A significant predictor of weight gain is the age at which women’s menopause begins. For example, a 2016 study published in Maturitas found that women who attained menopause before 51 years had less body fat [8].
Moreover, other factors may be involved in weight gain after menopause.
Women in their postmenopausal ages are generally less active than younger women. As such, they do not expend much energy, thus leading to a loss of muscle mass [9, 10].
Women experiencing menopause also have high fasting insulin levels and insulin resistance, which contribute to weight gain and increase the risk of heart disease [11].
Sleep problems during menopause
Menopause occurs when the ovaries stop producing progesterone and estrogen. We know that both hormones are essential in bodily processes affecting appetite, mood, sex drive, sleep, and more. For instance, progesterone may affect the breathing process, so low levels may cause sleep apnea and associated conditions.
Estrogen is involved in serotonin metabolism as well as the metabolism of other neurotransmitters that affect our sleep-wake cycle. Estrogen also maintains low body temperature at night, which is conducive to restful sleep. It is also worth mentioning that estrogen has antidepressant properties. When estrogen level is reduced, a woman may experience lower quality sleep, a higher body temperature, and poor mood.
Apart from that, the human sleep-wake cycle changes and becomes more inconsistent as a person ages. As a result, tiredness comes earlier, and we wake earlier in the morning, translating to less sleep overall. This also explains the high risk of insomnia in menopausal women [12].
The mood changes associated with menopause may be linked to hormonal fluctuations. But on the other hand, they may also be caused by other stressors during menopause. For example, caring for aging parents, empty nesting, and worries about old age may also be stressors for women.
Some women may also take meds due to aging symptoms or menopause, which may affect their sleep. In addition, body aches, joint pains, and bladder problems due to aging can also cause sleep problems.
Risk of osteoporosis during menopause
Preventing osteoporosis is a primary concern for women during menopause and post-menopause. Menopause accelerates bone loss and also increases the risk of osteoporosis in women. Studies indicate that at least 20% of bone loss may occur during these stages. And approximately 1 in 10 women above the age of 60 may be affected by osteoporosis globally.
One in two women who have attained menopause will have osteoporosis, and many will have a fracture at least once in their postmenopausal years. Fractures cause decreased mobility, function, and pain. In addition, fractures are associated with increased mortality and reduced quality of life.
It is important to note that no time is too late to be treated for osteoporosis. However, older women may respond better to early treatment.
A variety of treatments can help stop osteoporosis. The steps below can help to prevent bone deterioration.
Taking Calcium, and vitamin D
Calcium is vital for developing strong bones. Calcium also keeps your bones strong as you age. According to the National Institutes of Health (NIH), adults between the ages of 19 and 50 should get 1,100 milligrams of calcium daily.
Women over the age of 50 and all adults over the age of 70 should get no less than 1,200 milligrams each day. You may opt for supplements if you cannot get adequate calcium through natural food sources like kale, dairy products(cheese and yogurt), and broccoli. Calcium citrate and calcium carbonate are good calcium supplements.
The body makes vitamin D naturally when it is exposed to the sun. However, several factors influence the time it takes in the sun for the body to produce vitamin D. These factors include the time of the day, where you live, the environment, and your skin pigment.
The National Health Institute recommends that adults between the ages of 19 and 70 have a daily vitamin D intake of 600 international units (600 IU). People older than 70 should take up to 800 IU per day. But some people need more vitamin D3, up to 4,000-5,000 IU daily (Consult with your doctor before choosing the dose of vitamin D you should take).
Here’s an important point to note. If you are not getting enough vitamin D from food and sunlight, consider using a supplement.
You see, there are two vitamin D supplements: ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Vitamin D3 is the best. Research shows that vitamin D3 is more effective at raising blood levels of vitamin D than vitamin D2 [17, 18].
Taking Magnesium, and K2 supplements
Magnesium is an essential mineral that is involved in no less than 300 reactions in the body. Magnesium is also important for bone health. It is important to note that over 60% of magnesium is found in bone tissue.
Magnesium has a recommended daily intake of 310-320 mg per day for people between 19-30 years of age and 400-420 mg for people above 31 years of age. Magnesium needs are also slightly elevated during breastfeeding and pregnancy [19]. A study involving 51 post-menopausal women found that over 40% of women with osteoporosis had deficient levels of magnesium circulating in their blood [20].
Also, several studies involving adults have found that individuals who take high amounts of magnesium either through their supplements or diet have better bone mass density than those who consume low amounts of magnesium [21, 22].
Vitamin K2 is also known as menaquinone. Vitamin K2 has a protective effect on the bones. Studies have shown that poor intake of vitamin K2 is associated with low bone mass, fracture risk, and osteoporosis.
It is important to combine both magnesium and vitamin K2 when taking calcium for this reason: Magnesium helps to build healthy bones. It converts vitamin D into its active form, 1,25-dihydroxy-vitamin D3. On its part, vitamin K2 directly transports calcium from the blood into the bone tissue.
Prescription medications and bone-building agents
A group of medications known as bisphosphonates like Risedronate ibandronate, Alendronate, Pamidronate, ibandronate, and zoledronic acid can be taken as pills or injections intravenously. You need to take into consideration the side effects of these drugs. Consult with your doctor to see which one of these drugs is better for you. These medications have been shown to increase bone density, slow bone loss, and drastically reduce the risk of bone fractures.
According to a 2017 study published in the Journal of Bone Metabolism, bisphosphonates can minimize fractures due to osteoporosis by over 60 percent.
Include weight-bearing exercise in your fitness regimen
Exercise is vital for building strong bones and maintaining them. Exercise prevents bone loss and strengthens the bone. It also facilitates recovery when a person has a fracture.
Jogging, aerobics, walking, and dancing are examples of weight-bearing exercises.
Bioidentical hormone replacement
Estrogen replacement can help prevent osteoporosis, especially in women in the perimenopausal and menopausal stages of their life. The role of the hormone estrogen is to modulate bone metabolism and maintain skeletal bone density. Prevention of osteoporosis is one of the significant benefits of hormone replacement therapy in females, considering that a weaker skeleton can cause hip fractures.
Consult your healthcare to see if bioidentical hormone replacement is the right treatment for your case.
What's the endocrine link?
Osteoporosis is a technical term for “porous bones.” It is a progressive condition in which the bones weaken and are more likely to break or fracture. Menopause is a common cause of osteoporosis. During menopause, hormonal levels change to accommodate the changes that come with menopause.
Estradiol is one of the estrogen hormones produced naturally in the body. Therefore, estradiol’s effects manifest clearly in menopausal women. During this process, estradiol level reduces naturally as the ovaries no longer produce it, resulting in the cessation of menstrual cycles. This results in vaginal dryness, mood swings, night sweats, and hot flashes – the usual symptoms of menopause. In addition, over time, low estradiol levels can result in osteoporosis.
Hyperthyroidism and osteoporosis during menopause
If a woman has hyperthyroidism, the first step is to take care of the overactivity in the thyroid gland. Once you’ve reduced your thyroid hormone level to normal, the rate of bone loss will slow down, and the strength of your bone may improve.
However, it is essential to note that some people usually have persistent bone loss, whether they have a thyroid condition or not. Postmenopausal women have a very high risk of this. Suppose you’ve had hyperthyroidism that has not been treated for years or other risk factors for bone fractures and osteoporosis. In that case, conducting a bone mineral density scan within two to three years of your thyroid treatment will help assess your risk.
How bioidentical hormones can restore the sex hormones in menopause
Bioidentical hormones are synthetic hormones formulated to work like natural hormones (estradiol, progesterone, and testosterone). Taking these hormones can relieve the symptoms of unbalanced or low hormones, which is typical of menopausal or perimenopausal women.
Bioidentical hormones are used in the body in a process known as Bioidentical hormone therapy (BHRT). Progesterone, estrogen, and testosterone are the commonest bioidentical hormones. It is also important to check your levels of precursors hormones like DHEA and pregnenolone that will decrease after menopause.
Drug firms manufacture some forms of bioidentical hormones. The United States Food and Drug Administration has approved some types of bioidentical hormones. Other hormones are produced by compounded pharmacies based on the prescription by a healthcare provider.
Your healthcare provider may order blood tests to check your hormonal levels and follicle-stimulating hormone. The test for these hormones helps to confirm menopause and also detect signs of some pituitary disorders.
Your healthcare provider should also order additional tests to check the function of your thyroid (TSH, FT4, FT3, and thyroid antibodies) because hypothyroidism or hypothyroidism may share similar symptoms with menopause.
Taking hormone therapy is a decision you make under your healthcare provider’s guidance. Usually, this decision is made after weighing the benefits and risks of the treatment.
Menopause Relief without hormones
A drop in estrogen levels is the reason why women experience symptoms of menopause.
Estrogen typically binds to receptors on cell membranes. Upon binding, it activates the cellular process. Some of these cellular processes may be beneficial, while others may be detrimental.
Activating the ER-beta receptor benefits the brain, cardiovascular tissues, bone, and skin. This can improve menopausal symptoms.
On the other hand, activating the ER-alpha receptor can trigger undesirable growth in specific tissues, including the development of cancer cells.
Increased ER-alpha receptor activity is the primary cause of most ill effects of conventional hormone-replacement therapy [13].
For over three decades, researchers in Germany have been recommending the extract of the Siberian rhubarb plant for the safe treatment of these symptoms [14].
Preclinical studies have shown that these plant compounds have a stronger affinity for estrogen receptor-beta (ER-beta) compared to the potentially detrimental ER-alpha [15].
Siberian rhubarb extract did not activate ER-alpha in the study.
Siberian rhubarb extract is considered safe because of its ability to activate ER-beta rather than ER-alpha [16].
Tests to find out if you are in menopause and thyroid tests
Hormone tests
Your healthcare provider may recommend a blood test to determine your levels of Progesterone, Testosterone, Estrogen, and follicle-stimulating hormone levels. Your FSH levels will increase during menopause, while your estrogen, progesterone, testosterone, pregnenolone, and DHEA levels start decreasing during perimenopausal and menopausal women.
The anterior pituitary gland releases FHS in the first half of a woman’s menstrual cycle. FHS stimulates egg maturation as well as the production of estradiol.
Estradiol regulates the menstrual cycle and supports the female reproductive tract.
In addition to confirming menopause signs, this blood test can detect underlying pituitary disorders’ symptoms.
Recently, the FDA has approved a diagnostic test known as the PicoAMH Elisa test, which measures the level of anti-Mullerian hormone (AMH) in the blood. With AMH, your healthcare provider can determine when you’ll enter menopause, assuming you’re still in perimenopause.
Thyroid tests
T4 tests – Your thyroid gland produces 6% T3 and 94% T4. The blood has some proteins that bind T3 to T4 during circulation. With a total T4 test, your doctor can determine the aggregate level of the bound and free T4 hormone.
T3 test – A T3 test is reliable during a hyperthyroidism diagnosis. It may not be necessary for someone with menopause or hypothyroidism symptoms.
Free T3 test – Your doctor can also measure free T3. However, this test is rarely done because it is uninformative in most cases.
Thyroid antibody tests – Antibodies are usually released into the bloodstream by the immune system in a healthy body. These antibodies help to fight off bacteria, viruses, and other pathogens. The immune system considers the thyroid gland a foreign invader in most people with an overactive or underactive thyroid. As such, it will manufacture antibodies against cell proteins of the Thyroid. Thyroid antibody tests measure the levels of thyroid peroxidase and thyroglobulin antibodies. If you are experiencing overlapping symptoms of menopause and hypothyroidism, these antibody tests will help your doctor to make a conclusive diagnosis alongside others like T3, T4, and TSH.
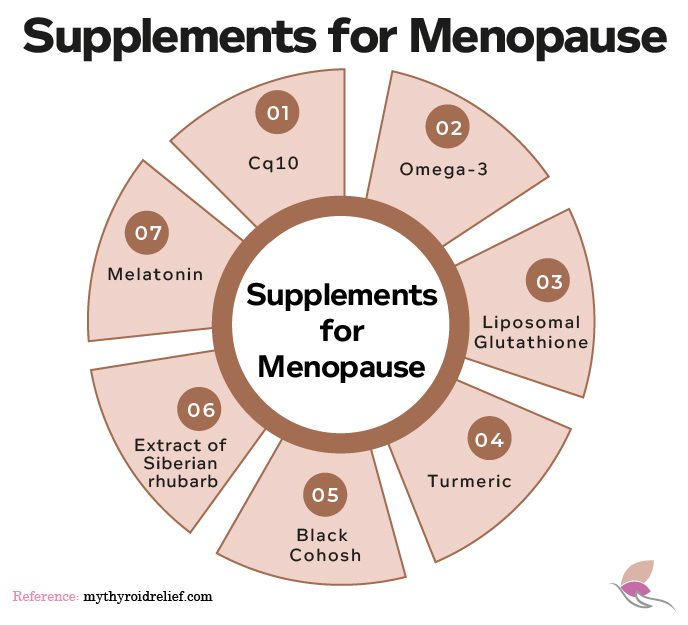
Vitamins and supplements you need to take to help you during menopause
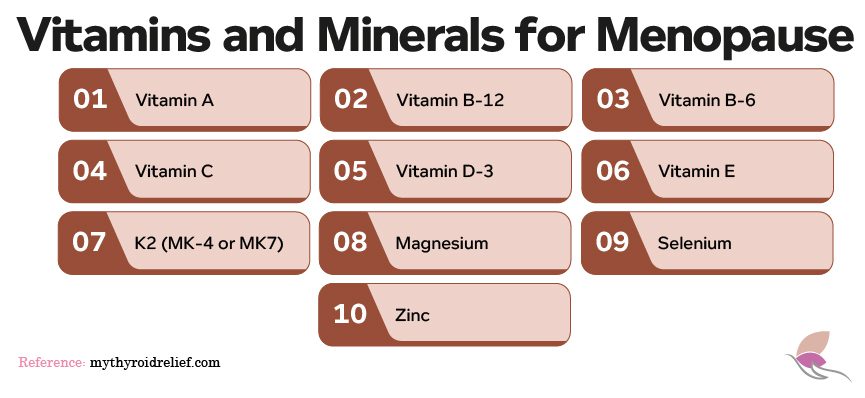
There are several supplements and vitamins on the market that can help ease the symptoms of menopause. However, one may be confused due to the many options in the market. As such, figuring out the best option can be challenging.
How to choose?
When choosing a multivitamin or supplement for menopause, you must consider the following factors:
Intended use. Most products in the market are formulated for the treatment of specific conditions associated with menopause. So, you should understand your health needs and choose a supplement with the ingredients to address your situation.
Quality ingredients. Choose supplements that are safe, strong, and pure. The ingredients in such a supplement should have been tested by a third-party organization or an independent laboratory.
Budget. You must evaluate your budget and check the price to know what fits your needs.
Dosage. Apart from the ingredients, you must consider the daily capsules you’ll have to take.
Consult your healthcare provider before using any supplement. They will guide you on whether a supplement is best for you.
Vitamins that will help minimize the symptoms of Menopause:
- Vitamin A
- Vitamin B-12
- Vitamin B-6
- Vitamin C
- Vitamin D-3,
- Vitamin E
- K2 as MK7
Supplements
- Cq10
- Magnesium
- Selenium
- Zinc
- Omega-3
- Lyposomal Gluthatione
Natural supplements for menopause symptoms
Since menopause is an entirely natural process, treatment is targeted at symptom management. The risk of side effects of some pharmaceutical drugs prompts the use of alternative therapies by many women.
Consult your healthcare provider before using any supplements for menopause.
Supplements commonly used to manage menopause include
When to see a healthcare provider
Many women suffer from menopause and hypothyroidism symptoms. Knowing more about your situation is the best option. Consult your healthcare provider if you are experiencing any symptoms of menopause or hypothyroidism, or both.
It is important to consult with a doctor (holistic) when you consider using bioidentical hormone replacement to increase your hormone levels and to disclose any symptoms you’ve been experiencing, especially weight changes, moodiness, irregular menstrual cycle, fatigue, and hot flashes, and memory problems.
Conclusion
Menopause and hypothyroidism have several overlapping symptoms. Not only do their effects overlap, but thyroid hormones and estrogen can influence each other and exacerbate symptoms.
Thyroid function is affected by the fluctuation of estrogen levels in the body after menopause. This can affects the thyroid glands’ ability to produce adequate triiodothyronine (T3) and thyroxine (T4) that the body needs to function correctly.
Hypothyroidism and hyperthyroidism, and other thyroid conditions can increase your risk of menopause-related complications, such as heart disease, insomnia, weight gain, and urinary tract infection.
Vitamins and supplements may help protect women during menopause from their symptoms due to lower levels of their hormones and also will improve bone density. For instance, calcium with vitamin D, magnesium, and vitamin K2 are vital for developing healthy bones. Vitamin D3, magnesium, and vitamin K2 can enhance calcium absorption and the body’s ability to use it effectively, avoiding the risk of having it deposited in the arteries.
Bisphosphonates drugs have been shown to increase bone density, slow bone loss, and drastically reduce the risk of bone fractures, but they have side effects you need to consider before choosing any of these drugs.
It is crucial to have blood tests of our sex and thyroid hormones before and after menopause to monitor our levels to take adequate medical measurements to avoid osteoporosis and resolve our unbalanced hormone symptoms.
Sometimes, these tests are followed up with imaging tests of the neck to visualize the thyroid gland. Suppose blood tests do not indicate any thyroid hormone dysfunction; your symptoms may be caused by perimenopause, menopause, or an underlying medical issue that alters the hormones.
Hormone levels can be restored through the use of bioidentical hormones. Bioidentical hormones are synthetic hormones that work like natural hormones (estradiol, progesterone, and testosterone). Also, it is essential to measure your levels of Pregnenolone and DHEA.
Taking these hormones can relieve the symptoms of unbalanced or low hormones and improve bone mass in perimenopausal and menopausal women.
It would help if you had a holistic healthcare provider who listens and can guide you on getting an accurate diagnosis and an effective treatment plan.
References
- Tunbridge WMG, Evered DC, Hall R. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol. 1977;7:481–493
- Vanderpump MPJ, Tunbridge WMG, French JM, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol. 1995;43:55–68
- Badawy, A., State, O., & Sherief, S. (2007). Can thyroid dysfunction explicate severe menopausal symptoms?. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology, 27(5), 503–505. https://doi.org/10.1080/01443610701405812
- Schindler A. E. (2003). Thyroid function and postmenopause. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 17(1), 79–85.
- Santin, A. P., & Furlanetto, T. W. (2011). Role of estrogen in thyroid function and growth regulation. Journal of thyroid research, 2011, 875125. https://doi.org/10.4061/2011/875125
- Tuchendler, D., Bolanowski, M. The influence of thyroid dysfunction on bone metabolism. Thyroid Res 7, 12 (2014). https://doi.org/10.1186/s13044-014-0012-0
Oh wow, I didn’t realise that you could experience the symptoms of menopause for at least a decade. That is something I hope doesn’t happen when I get to this stage. It’s not pleasant from what I hear.
Hello Melanie! It is important to note that menopause affects each woman differently, and some women may not experience any symptoms at all.
I didn’t know there was a connection between menopause and thyroid. I remember how much my mother struggled with it, and I hope that I am not inherit the same genes. It’s definitely a very difficult time in a woman’s life.
Hi Joanna,
Certainly, menopause and thyroid health can be interconnected, especially if there’s a family history. While genetics can play a role, staying proactive with regular check-ups and discussions with healthcare providers is essential. Remember, knowledge is power, and being informed about potential health risks can help you make informed decisions and take appropriate steps to maintain your well-being. Feel free to reach out if you have any questions or need support. Take care!
I have never thought about the menopause and the thyroid having a link, but reading this post, a lot clicks into place!
Hi Rachel,
It’s fascinating how interconnected our organs, glands, etc can be. I’m glad the post helped shed light on the connection between menopause and thyroid issues for you. Feel free to reach out if you have any more questions or want to explore related topics further. I’m here to help!
I have never thought about the menopause and the thyroid having a link, but reading this post, a lot clicks into place! Thanks for sharing.
I wouldn’t of thought there was a connection until reading this . Some great informative information x
Hi Kira! I’m glad to hear that you found my response informative! The human body is a complex system, and there are often connections between different parts that we might not immediately think of.
What a thorough guide about the connection between menopause and the thyroid. I didn’t realise that menopause could start that early, it’s actually kind of scary x
Hello! I’m glad you found my post helpful!
Hi Rhian Westbury,
I’m glad you found the guide informative! Yes, it can be surprising to discover that menopause can begin earlier than expected. It’s a natural part of life, and while it may seem a bit daunting, there are many ways to manage and navigate this stage with confidence and good health. If you have any more questions or concerns, feel free to ask! Thanks for reading our blog.
“Thank you, Rhian! We appreciate your kind words. Yes, the connection between menopause and the thyroid can be quite surprising, and it’s always good to be informed. Thanks for visiting our blog.